Cervical cancer:
Cervical cancer is the third most common gynecologic malignancy in the United States [4,13]. Almost half of the cases of invasive cervical cancer occur in patients under the age of 35 years [13]. Risk factors for cervical carcinoma include: Multiple sex partners, condyloma (more than 90% of squamous cell cancers of the cervix contain human papilloma virus DNA [3]), and herpes. About 85-95% of cervical carcinomas are of the squamous cell variety, and adenocarcinoma accounts for the remaining 5-15%. Predictors of disease free survival in patients with early stage cervical carcinoma include tumor size, depth of invasion, and invasion of the lymphatic or vascular space. The parametrium is the connective tissue between the leaves of the broad ligament. It abuts the uterus, cervix, and proximal vagina [2]. Laterally, it extends to the pelvic sidewall [2]. The distal ureter is in the parametrium [2]. The probability of parametrial invasion is only 6% for tumors less than 2 cm in diameter, but increases to 28% for tumors greater than this size. Cervical carcinoma most commonly metastasizes to regional lymph nodes and the extent of nodal involvement is an important prognostic indicator [4]. The presence of metstases is directly related to the size of the tumor.
The 5-year survival for patients in whom cervical cancer is detected early is about 91% [3]. For lesions over 4cm in size, metastases are found in 36% of cases, while for lesions less than 3 cm in size, metastases are present in 22% of cases. Additionally, 5 year survival decreases from 84% to 66% as the size of the tumor grows from 3 cm to 4 cm. At surgery, the presence or absence of nodal metastases impacts on patient survival. For IB disease, survival is 85-95% for patients with negative nodes at surgery, but drops to 45-55% for those with positive nodes [2,4]. Lymphatic spread from cervical tumors is initially to the parametrial nodes [4]. From the parametrial nodes, the tumor may extend laterally to the external iliac nodes, to the hypogastric nodes that lie along the internal iliac vessels, or posteriorly along the uterosacral ligaments to the lateral sacral and sacral promontory nodes [4]. The presence of para-aortic lymph node metastases significantly worsens prognosis [7]. Bone metastases occur infrequently [13].
Accurate determination of the stage of disease is important as therapy is based upon stage. The two features of disease extent that commonly define treatment choice are parametrial tumor extension and lymph node metastases [17]. Patients with clinical stage IB or IIA cancer can be treated with either radical hysterectomy and pelvic lymphadenectomy, or with radiation therapy. For patients with tumor extending to the parametria (Stage IIB) or beyond, treatment consists of radiation and/or chemotherapy. Therefore, the important decision in staging is in distinguishing stage IIA from IIB [2]. Unfortunately, a large percentage of patients can be clinically understaged [17]. Up to 24% of patients with clinically staged FIGO IB cervical cancer are found to have more advanced disease at surgery [17].
PET imaging:
Because the cervix is in close proximity to the urinary bladder, FDG activity in the bladder may mask the primary, metastatic, and recurrent lesions [12]. For imaging patients with cervical carcinoma, a foley catheter and continuous bladder irrigation are useful to clear urinary activity [7,12]. Lasix also aids in clearing renal and ureteral activity [7].
Primary lesion:
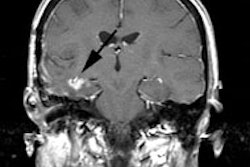
FDG is taken up by about 91% of primary cervical tumors [6]. Uptake has been correlated with over-expression of the Glut-1 glucose transporter [8]. Note that increased uptake can be seen within the endometrium above a cervical tumor and does not necessarily reflect tumor extension [9].
Nodal Metastases:
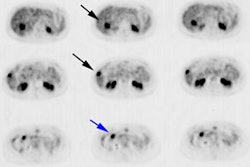
Definition of lymph node status is one of the most important prognostic factors in cervical cancer [12]. In one study comparing MR imaging with FDG PET, PET improved the sensitivity in detection of lymph nodes metastases from 50-73% to 83-91% [6]. In another study, metastatic para-aortic lymph nodes were identified with a sensitivity of about 82% [7]. In a prospective evaluation of patients with clinical stage IA or IB cervical cancer scheduled for treatment with radical hysterectomy and pelvic lymph node dissection, PET/CT showed a node based sensitivity of 72% for the detection of metastatic disease (sensitivity was 100% for all nodes larger than 5 mm) [14]. Overall patient based detection of lymph node involvement is sensitivity 73-77%, specificity 56-97%, PPV 92%, NPV 89%, and accuracy 89% [14,17].
Findings on the PET exam can result in a change in planned treatment in 21% of patients [7]. Lymphoscintigraphy may aid in directing appropriate lymph node sampling when node dissection is to be performed in early grade patients [13].
Recurrent disease:
Approximately 30% of cases of cervical cancer will recur following treatment for patients with stage IB or higher disease- often with a combination of local and distant metastases [5,16]. The majority of recurrences occur within the first 2 years after completion of therapy- about 60% of recurrences occur within two years and 90% within 5 years [6,15]. Stage and lymph node status at the time of diagnosis are strong predictors of disease recurrence [15]. Patients with the greatest risk of recurrence are those with Stage IIb and Stage III cancer [5]. The most common sites for recurrence are the vaginal cuff, cervix, parametrium, and pelvic side wall [6]. Early detection of recurrence and institution of salvage treatment can result in improved patient survival [15]. However, curative therapy is futile in the presence of distant metastases [16].
In a prospective evaluation of 249 patients with no evidence of cervical cancer following treatment, FDG PET imaging identified recurrence in 11% of patients [5]. The sensitivity and specificity of FDG PET for detection of early recurrence were 90% and 76%, respectively [5]. The sensitivity was lower for detection of lung, retrovesical nodes, and para-aortic nodes [5].
One critical issue in the evaluation of recurrent disease is distinguishing post-radiation changes from recurrent tumor which is not always possible with conventional imaging [6]. PET imaging can help to clarify the diagnosis of clinically suspected recurrence [16]. In patients with clinically equivocal recurrences FDG PET has a sensitivity of 92%, a specificity of 93%, a PPV of 96%, and a NPV of 87% [16]. PET findings can change the planed treatment in about 50% of cases [16]. In these patients, a positive PET also carried prognostic significance with overall decreased survival compared to patients with negative PET exams [16].
Another group of patients that can benefit from PET imaging are those with a prior complete response to therapy who present with rising tumor markers (squamous cell carcinoma antigen) and negative conventional imaging exams [13]. PET imaging can detect recurrent disease in up to 94% of these patients [13]. Early detection and early institution of appropriate therapy and lead to improved survival [13].
For the detection of recurrent cervical cancer, cumulative data indicate that FDG PET has a mean sensitivity and specificity of approximately 95% and 84%, respectively [10]. The mean diagnostic accuracy is about 88% [10]. Overall, PET is superior to conventional imaging modalities for the detection of metastatic recurrent cervical cancer [11]. The findings on the PET exam can affect patient management in 23-65% of patients [10,16].
Prognosis/Monitoring response to therapy:
Following primary treatment, PET imaging can provide additional prognostic information compared to conventional imaging. A complete metabolic response is associated with a very good survival outcome [15]. FDG uptake at sites of primary treatment or at new locations is a significant negative prognostic indicator [10,15]. Two-year progression free survival is 64% in CT-negative/PET-negative patients, 18% in CT-negative/PET-positive patients, and 14% in CT-positive/PET-positive patients [12]. In another study, 2 year progression free survival was 80% in PET negative patients, compared to only 40% in PET positive patients [12]. A prospective study of patients with cervical cancer found a complete metabolic response on PET imaging performed 8-16 weeks following completion of therapy was associated with a 3 year progression free survival of 78%; a partial metabloic response with a survival rate of 33%; and the development of progressive disease with a 0% survival rate [15].
Limitations of FDG PET imaging in cervical carcinoma:
Activity within the ureters may be misinterpreted as lymph node metastases [7].
REFERENCES:
(1) Radiology 1998; Scheidler J, et al. Parametrial invasion in cervical carcinoma: Evaluation of detection at MR imaging with fat suppression. 206: 125-129
(2) Radiographics 2001; Panni HK, et al. CT evaluation of cervical cancer: spectrum of disease. 21: 1155-1168
(3) Radiographics 2003; Szklaruk F, et al. MR imaging of common and uncommon large pelvic masses. 23: 403-424
(4) AJR 2003; Kaur H, et al. Diagnosis, staging, and surveillance of cervical carcinoma. 180: 1621-1632
(5) J Nucl Med 2003; Ryu SY, et al. Detection of early recurrence with 18F-FDG PET in patients with cervical cancer. 44: 347-352
(6) AJR 2003; Kaur H, et al. Diagnosis, staging, and surveillance of cervical carcinoma. 180: 1621-1632
(7) J Nucl Med 2003; Ma SY, et al. Delayed 18F-FDG PET for detection of paraaortic lymph node metastatses in cervical cancer patients. 44: 1775-1783
(8) J Nucl Med 2004; Yen TC, et al. 18F-FDG uptake in squamous cell carcinoma of the cervix is correlated with glucose transporter 1 expression. 45: 22-29
(9) J Nucl Med 2004; Lerman H, et al. Normal and abnormal 18F-FDG endometrial and ovarian uptake in pre- and postmenopausal patients: assessment by PET/CT. 45: 266-271
(10) J Nucl Med 2004; Belhocine TZ. 18F-FDG PET imaging in posttherapy monitoring of cervical cancers: from diagnosis to prognosis. 45: 1602-1604
(11) J Nucl Med 2004; Yen TC, et al. Defining the priority of using 18F-FDG PET for recurrent cervical cancer. 45: 1632-1639
(12) Radiol Clin N Am 2004; Kumar R, Alavi A. PET imaging in gynecologic malignancies. 42: 1155-1167
(13) J Nucl Med 2005; Pandit-Taskar N. Oncologic imaging in gynecologic malignancies. 46: 1842-1850
(14) Radiology 2006; Sironi S, et al. Lymph node metastasis in patients with clinical early-stage cervical cancer: detection with integrated PET/CT. 238: 272-279
(15) JAMA 2007; Schwarz JK, et al. Association of posttherapy positron emission tomography with tumor response and survival in cervical carcinoma. 298: 2289-2295
(16) J Nucl Med 2008; van der Veldt AAM, et al. Clarifying the diagnosis of clinically suspected recurrence of cervical cancer: impact of 18F-FDG PET. 49: 1936-1943
(17) AJR 2009; Pandharipande PV, et al. MRI and PET/CT for triaging stage IB clinically operable cervical cancer to appropriate therapy: decision analysis to assess patient outcomes. 802-814