Introduction
Physicians use the term "grade" to describe the appearance of thin slices of cancer tissue when it is observed under a microscope. In the case of prostate cancer tissue, the most common system used in the USA to grade the appearance of this tissue is called the Gleason grading system, after the physician who first described this system.The Gleason grading system is not the only grading system in use around the world. However, because it is the one most commonly used in the USA, it is the one we will try to explain here. If your physician talks to you about the grade of your prostate cancer, you may want to ask if it is the Gleason grade that he or she is referring to.
The Gleason grade is one of several pieces of information determined by the pathologist who examines the biopsy specimen taken from the prostate. Readers wishing to understand more about the role of the pathologist in the diagnosis of prostate cancer may wish to read the article entitled ""The pathologic examination of prostate tissue", which addresses this topic in detail, and which also explains the importance to the patient of receiving a copy of his pathology report.
The Gleason system is based exclusively on the architectural pattern of the glands of the prostate tumor. It evaluates how effectively the cells of any particular cancer are able to structure themselves into glands resembling those of the normal prostate. The ability of a tumor to mimic normal gland architecture is called its differentiation, and experience has shown that a tumor whose structure is nearly normal (well differentiated) will probably have a biological behavior relatively close to normal -- that is not very aggressively malignant.
The principle is fairly simple, and Gleason grading from very well differentiated (grade 1) to very poorly differentiated (grade 5) is usually done for the most part by viewing the low magnification microscopic image of the cancer. There are important additional details which require higher magnification, and an ability to accurately grade any tumor is achieved only through much training and experience in pathology.
The five Gleason grades
Dr. Gleason has provided a conceptual diagram (oversimplified) in Figure 1 to show the continuum of deteriorating cancer cell architecture, and the four dividing lines along this continuum which he discovered are able to identify patients with significantly different prognosis derived from a study which included 2,900 patients.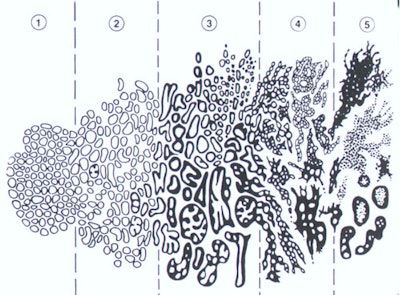
Figure 1: This illustration shows Dr Gleason's own simplified drawing
of the five Gleason grades of prostate cancer. Grade 1 appears on the far
left and grade 5 on the far right. Adapted from Gleason DF. The Veteran's
Administration Cooperative Urologic Research Group: histologic grading
and clinical staging of prostatic carcinoma. In Tannenbaum M (ed.) Urologic
Pathology: The Prostate. Lea and Febiger, Philadelphia, 1977; 171-198.
We would like to thank Dr John McNeal of the Department of Urology, Stanford University School of Medicine, for kindly assisting us in developing this information.
Gleason Grades 1 and 2: These two grades closely resemble normal prostate.
They are the least important grades because they seldom occur in the general
population and because they confer a prognostic benefit which is only slightly
better than grade 3. Both of these grades are composed by very pale glands
which grow closely together. In grade 1 they form a compact mass; in grade
2 they are more loosely aggregated, and some glands wander (invade) into
the surrounding muscle (stroma).
Gleason Grade 3: This is the most common grade by far and is also considered
well differentiated (like grades 1 and 2). This is because all three grades
have a normal "gland unit" like that of a normal prostate; that is, every
cell is part of a circular row which forms the lining of a central space
(the lumen). The lumen contains prostatic secretion like normal prostate,
and each gland unit is surrounded by prostate muscle which keeps the gland
units apart. In contrast to grade 2, wandering of glands (invading) into
the stroma (muscle) is very prominent and is the main defining feature.
The cells are dark rather than pale and the glands often have more variable
shapes.
Gleason Grade 4: This is probably the most important grade because it is fairly common and because of the fact that if a lot of it is present, patient prognosis is usually (but not always) worsened by a considerable degree. Here also there is a big jump in loss of architecture. For the first time, we see disruption and loss of the normal gland unit. In fact, grade 4 is identified almost entirely by loss of the ability to form individual, separate gland units, each with its separate lumen (secretory space). This important distinction is simple in concept but complex in practice. The reason is that there are a variety of different-appearing ways in which the cancer's effort to form gland units can be distorted. Each cancer has its own partial set of tools with which it builds part of the normal structure. Grade 4 is like the branches of a large tree, reaching in a number of directions from the (well differentiated) trunk of grades 1, 2, and 3. Much experience is required for this diagnosis, and not all patterns are easily distinguished from grade 3.
Gleason Grade 5: Gleason grade 5 is an important grade because it usually predicts another significant step towards poor prognosis. Its overall importance for the general population is reduced by the fact that it is less common than grade 4, and it is seldom seen in men whose prostate cancer is diagnosed early in its development. This grade too shows a variety of patterns, all of which demonstrate no evidence of any attempt to form gland units. Figure 7 shows only a sea of black nuclei with no pattern. The variety of different appearances is less than for grade 4 because there are fewer ways to do nothing! This grade is often called undifferentiated, because its features are not significantly distinguishing to make it look any different from undifferentiated cancers which occur in other organs.
The combined Gleason score or Gleason sum
When a pathologist looks at prostate cancer specimens under the microscope and gives them a Gleason grade, he or she in fact will always try to identify two most common architectural tumor patterns and assign a Gleason grade to each one. There may be a primary or most common pattern and then a secondary or second most common pattern which the pathologist will seek to describe for each specimen; alternatively, there may often be only a single pure grade. Approximately 85% of prostate cancers are multifocal [1].In developing his system, Dr Gleason discovered that by giving a combination of the grades of the two most common patterns he could see in any particular patient's specimens, he was better able to predict the likelihood that that particular patient would do well or badly. Therefore, even though it may seem confusing, the Gleason score which a physician usually gives to a patient is actually a combination or sum of two numbers. These combined Gleason sums or scores may be determined as follows:
The lowest possible Gleason score is 2 (1 + 1), where both the primary and secondary patterns have a Gleason grade of 1 and therefore when added together their combined sum is 2.
Very typical Gleason scores might be 5 (2 + 3), where the primary pattern has a Gleason grade of 2 and the secondary pattern has a grade of 3, or 6 (3 + 3), a pure pattern.
Another typical Gleason score might be 7 (4 + 3), where the primary pattern has a Gleason grade of 4 and the secondary pattern has a grade of 3.
Finally, the highest possible Gleason score is 10 (5 + 5), when the primary and secondary patterns both have the most disordered Gleason grades of 5.
What does the Gleason score mean?
The grade of a prostate cancer specimen is very valuable to doctors in helping them to understand how a particular case of prostate cancer can be treated. In general, the time for which a patient is likely to survive following a diagnosis of prostate cancer is related to the Gleason score. The lower the Gleason score, the better the patient is likely to do. Cancers with a Gleason score of 6 or lower are considered well differentiated and associated with a good prognosis [1]. Cancers with a Gleason score of 8-10 have the worst prognosis and the highest risk for recurrence [1]. Tumors with a Gleason score of 7 have a variable prognosis [1].However, remember that prostate cancer is a very complicated disease. People with low Gleason scores have been known to fare poorly and men with high Gleason scores have been known to do well. General principles do not always apply to individual patients.
By combining the patient's Gleason score with his PSA level and the clinical stage estimated by the physician, it is possible to use the Partin coefficient tables to estimate the likelihood that that patient has localized or locally advanced prostate cancer of different types.
REFERENCES:
(1) AJR 2009; Kelloff GJ, et al. Challenges in clinical prostate cancer: role of imaging. 192: 1455-1470