Radiologists play a key role in steering the right patients into CT screening -- and the wrong patients away from it -- according to researchers from the University of California, Los Angeles. But when patients are sold on the exams, the doctors' advice may be falling on deaf ears.
At the 2002 RSNA meeting in Chicago, Dr. Carol Wu presented a study of screening referral patterns at UCLA. Her group found that physician-referred patients had far more screening-detected disease than patients who had decided on the scans by themselves. The trend persisted despite radiologists' extensive counseling of low-risk patients against the screening exams.
Wu, along with Dr. Jonothan Goldin and colleagues, retrospectively examined the records of 1,631 asymptomatic patients who had undergone CT of the chest and abdomen, DEXA bone-density screening, coronary artery calcium (CAC) screening, and/or ultrasound of the carotid arteries at the community-based center over the course of 16 months.
Out of 1,631 screening patients, 82.5% were physician-referred (PR) and 17.5% self-referred (SR), Wu said. The self-referred patients were much more likely to ask for whole-body CT exams, while physicians were likelier to order more goal-oriented studies such as CAC, Wu said.
"We noticed a significant difference in frequency of positive findings (among PR patients) that required further physician follow-up, such as (for) pulmonary nodules, elevated coronary artery calcium score, and renal masses," Wu said. "More than 50% of the SR patients received noncontrast lung CT or noncontrast abdominal CT. A much smaller percentage of the physician-referred patients received these studies."
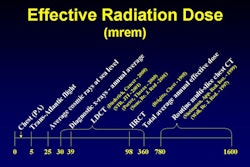
SR patients had slightly fewer noncalcified lung nodules than PR patients, and were likelier to have a coronary artery calcium score of zero. Conversely, PR patients were likelier to have CAC scores higher than 400 (p<0.05), which are associated with an increased risk of coronary events. Finally, SR patients received a higher average radiation dose (3 to 5 mSv) than PR patients (1.5 to 3 mSv).
"We found that self-referred and physician-referred patients have different motivations for screening tests," Wu concluded. "Physician-referred patients are more likely to (undergo) goal-oriented studies and therefore lower radiation exposure and find more potentially significant results."
At her group's screening facility, the radiologists took the time to individually counsel self-referred patients against unnecessary tests, Wu said.
"For example, if a patient comes in (with) no smoking history, and no asbestos exposure, then (he is) counseled by the radiologist to not have the lung study done. However, at most other facilities, where self-referred patients are not actively counseled against unnecessary studies, we would expect the difference between physician-referred and self-referred patients to be even larger than what we found."
Still, an audience member at Wu’s presentation questioned whether having the radiologists counsel patients at length was a good use of physician time.
By Eric BarnesAuntMinnie.com staff writer
January 3, 2003
Related Reading
CT screening centers: Is there a right way to start one?, November 12, 2002
Why CT lung cancer screening will (and won't) work, November 11, 2002
Whole-body CT: Radiology to the people?, October 2, 2002
Referring physicians reserve perfusion imaging for sickest patients, September 30, 2002
Primary care reminders reduce x-ray requests, September 27, 2002
Copyright © 2003 AuntMinnie.com