Applying the lowest feasible CT dose to pediatric imaging is a complex undertaking that is aided only imperfectly using standard patient-stratification techniques based on age, height, and weight. In a bid to develop more accurate patient-stratification methods to optimize the protocols used for chest, abdominal, and pelvic studies in children, researchers from the M.D. Anderson Cancer Center and University of Texas Medical School in Houston, and Toledo Hospital in Toledo, OH, used child-sized acrylic phantoms rigged with dosimeters for their study.
The overexposure of pediatric patients can be easily overlooked, the authors wrote in the American Journal of Roentgenology, and even though several methods are available to determine the optimal protocol based on patient size, the resulting radiation dose often varies widely from patient to patient (AJR, April 2004, Vol. 182:4, pp. 849).
Typically, a combination of patient age, height, and weight are used to set CT scanning parameters, wrote study authors Dr. Diana Cody, Dr. Donna Moxley, Dr. Kerry Krugh and colleagues.
"At our institution, we have recognized that our pediatric patient population does not lend itself well to this approach," they wrote. "Our patients' body shapes are often affected by their disease or treatment or both, and they frequently present as either emaciated or bloated, neither of which would be appropriately compensated by an age, height, and weight approach to tailoring CT scanning protocols. Haaga et al...have advocated the use of a patient's diameter to determine parameters such as x-ray tube current. The optimal variable to use for this protocol assignment would be the cross-sectional area presented to the scanning plane. The display field of view used for the image reconstruction process is a reasonable surrogate for cross-sectional area."
The radiologists have learned to track the display field of view carefully in their institution in order to ensure consistent spatial scaling (magnification) between scans in the same patient. In their study, they deployed one adult-sized and three child-sized acrylic phantoms (representing one, five, and 10-year-olds) to examine the CT dose effects of the altered exposure parameters.
The phantoms were scanned in axial mode (to avoid relative over- or underexposure of the skin-dose surface monitors on the phantoms) using a LightSpeed scanner (GE Healthcare, Waukesha, WI) at 4 x 5-mm collimation, and varying mAs and kVp settings. Calibration factors were used to convert the output values to exposure on the ion chamber scale at 80, 100, 120, and 140 kVp.
"The skin dose monitor measurements obtained at the surface of the anthropomorphic phantoms at 120 kVp were compared with the results using both 16-cm and 32-cm-diameter CT dose-index phantoms and a standard CT pencil ion chamber with the same acquisition parameters (peak kilovoltage, milliampere, and time)," they wrote.
The skin dose monitors were calibrated using a standard CT ion chamber and electrometer exposed in air at the isocenter of the CT scanner with several technique factors. Calibration in air was used to convert the skin dose monitor data to the same scale as a standard CT ionization chamber dosimeter. And an f factor was used to convert the tissue dose (0.93 c/Gy/R) to more closely match the entrance dose measurement obtained using the phantoms [(CT dose indexp = (ICp) (0.93 cGy /R) (100 mm) / (1,000 mR/R) (20-mm overall beam width)]. Image noise values on axial 5-mm-thick phantom images were obtained to measure image quality, the authors wrote.
The study found that peripheral CT dose index (CTDI) values obtained with standard 16-cm acrylic phantoms underestimated the surface dose compared with the levels detected on all three pediatric phantoms by less than 10% of the CT surface dose measurements for both adult and child phantoms in chest and abdominopelvic scan protocols.
The CTDI for the 16-cm diameter acrylic phantom measurements overestimated the adult phantom surface dose by approximately 15%-20% for the chest exam; the overestimation was approximately 30% for the corresponding abdominopelvic exam. Using the 32-cm acrylic phantom, the CTDI underestimated the adult phantom surface dose by approximately 20%-35% for both chest and abdominopelvic scanning protocols, the authors wrote.
"As expected, the dose to the pediatric anthropomorphic phantoms was considerably higher than the adult dose for the same CT scanning technique.... The dose per unit milliampere-second for smaller patients was 1.6-1.7 times greater than that for an adult."
Meanwhile, noise in the abdominopelvic images was significantly greater than in the chest images, suggesting that chest imaging protocols in children should be designed with comparatively lower technique factors, they wrote. The noise in the child phantom images was generally one-third to one-half that of the noise in the adult phantom using the same exposure parameters.
Sample protocols
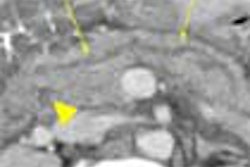
The optimized protocols were later applied to patients, including, for example, abdominopelvic imaging of a four-year-old boy with stage V renal Wilms’ tumor. Diagnostic-quality images were obtained using 100 kVp, 128 mAs (160 mAs and 0.8 sec), 23-cm field of view, 4 x 5-mm detector configuration, and pitch of 1.5. The study was acquired with approximately 18 mGy, representing a 40% dose reduction from the standard protocol, the authors wrote.
In a 21-month-old boy with cervical neuroblastoma, chest CT images were obtained at 80 kVp and 160 mAs, with 0.5-sec. rotation, 4 x 5-mm detector configuration, pitch 1.5, 5-mm slice thickness, and 21-cm field of view. Beam-hardening artifacts in the bony shoulder region led the group to increase the recommended kVp to 100 in follow-up imaging.
According to resulting sample protocol charts, chest CT for an approximate patient size represented by a 6-9 year-old would be optimally acquired at 100 kVp, 70 mAs, 0.8-sec. rotation speed (table travel 11.25 mm per rotation), pitch 0.75, 7.5-mm slice thickness, for a 24-26-cm display field of view on the LightSpeed scanner.
Abdominopelvic images for the same patient would optimally be acquired at 100 kVp, 130 mAs, 0.8-sec. rotation speed (table travel 30 mm per rotation), pitch 1.5, 7.5 mm slice thickness, for a 27-29-mm display field of view on the LightSpeed scanner.
When designing protocols it is important to use the fastest available rotation speed for pediatric patients in order to minimize patient motion artifacts, the authors noted.
"Our CT dose index approach yielded values that were within approximately 10% of the measured entrance exposure values for the pediatric phantoms for both chest and abdominopelvic CT examination protocols...," they wrote. "This study effectively validated the CT dose index method for use in pediatric subjects when the 16-cm-diameter acrylic phantom was used."
The researchers said they were somewhat surprised to find that the 16-cm-diameter acrylic CTDI phantom estimated the entrance dose measurements to the anterior midline of the adult phantom more accurately than did the standard 32-cm CTDI phantom. But the 32-cm CT dose index values offered a better estimate of the lateral adult phantom surface dose results than the 16-cm CTDI phantom.
"Any image-optimization process should include a careful evaluation of image quality; we have used the image-noise parameter as our primary end point in this respect. Other parameters such as contrast-to-noise ratio might have been more useful, but the limited internal anatomic structural detail of these anthropomorphic phantoms would have made (these) values...irrelevant to clinical applications."
The group concluded that acceptable image quality can be achieved by reducing adult scanning parameters to equivalent children’s settings on the basis of constant image noise, resulting in skin dose reductions of 60%-90% relative to adult settings.
"We found that the dose per unit milliampere-second on CT at constant scanning parameters can vary with subject size by greater than a factor of 1.7, and that the associated image-noise value for a given technique can vary with subject size by a factor of up to 3.3," they wrote. "Parameters other than age, weight, and height, such as display field of view, can also be used successfully to stratify pediatric CT protocol parameter ranges."
By Eric BarnesAuntMinnie.com staff writer
April 21, 2004
Related Reading
Pediatric CT won't stop growing, but dose can be minimized, May 8, 2003
High pitch, thin sections can optimize MDCT protocols, August 22, 2004
Radiologists offer new guidance on reducing CT radiation dose, August 14, 2004
Ask questions to optimize MDCT protocols, July 11, 2003
Copyright © 2004 AuntMinnie.com