Pancreas divisum is a congenital pancreatic anomaly that occurs when the ductal systems of the ventral and dorsal pancreatic ducts fail to fuse in utero. The result is a dominant dorsal duct, meaning that most or all pancreatic secretions enter the duodenum through the dorsal duct and minor papilla.
While the condition is most often asymptomatic, in some patients it can produce abdominal pain, or even pancreatitis. As a result, doctors consider pancreas divisum to be something worth knowing about, especially when presented with unexplained abdominal pain.
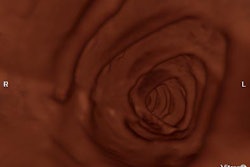
The gold standard for diagnosis has been the invasive ERP, or endoscopic retrograde pancreatography; CT’s sensitivity has been considered to be too low for general clinical use. But a new study presented at the 2004 European Congress of Radiology in Vienna found that, properly performed, noninvasive contrast-enhanced thin-section MDCT can also do an excellent job of diagnosing the condition.
According to radiologists from Boston University Medical Center, thin-section MDCT was less invasive than the gold standard test, and less expensive than MRI, with or without the use of secretin.
"As we know, pancreas divisum is a relatively common anomaly, and it’s found, they tell us, in somewhere between 4% and 8% of the population," said Dr. Brian Lucey, an assistant professor of radiology at Boston University School of Medicine. "There’s always a little controversy about the significance of pancreas divisum and whether or not it causes problems. But I think the general agreement at this stage is that it can be related to some sort of chronic abdominal pain, and occasionally cause pancreatitis. So therefore it is an important entity."
Lucey, along with lead investigator Dr. Jorge Soto and Dr. Joshua Stulhfaut, examined 41 consecutive patients (24 men, 17 women) who underwent both ERP and contrast-enhanced MDCT of the pancreas within 1 to 75 days (mean 19 days) after getting ERP as the first exam. All of the patients had been referred for the evaluation of abdominal pain.
Following intravenous administration of 100 mL of intravenous contrast material (320 mg/ml iohexol at 3 ml/sec., scan delay 40-60 seconds) the radiologists acquired MDCT images of the pancreas on an MX 8000 four-row multidetector-row scanner (Philips Medical Solutions, Andover, MA) using collimation of 3.2 mm, 3-mm reconstruction intervals, 140 kVp, and mAs of 200-250. "The 2D multiplanar reformats with the curved array are actually very useful for displaying the pancreatic duct, and the curved duct can be traced quite clearly on the curved-array formats," Lucey said.
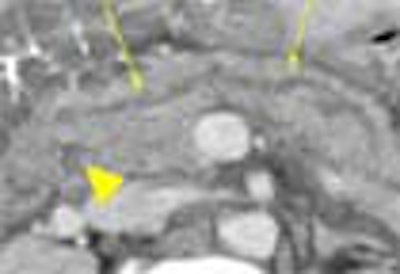
Two radiologists working independently reviewed the images on a PACS workstation, with the aid of 2D and 3D reformatting, and cine mode function. Diagnostic results and statistical measurements were calculated for each observer. The presence of the dominant dorsal duct sign was used to diagnose pancreas divisum, Lucey said.
The diagnosis was made "if we could trace the dorsal duct through the tail of the gland through the body of the gland and into the anterior aspect of the head, draining into the minor papilla...and if we could locate the ventral duct draining into the major papilla; or if the ventral duct was not seen, the caliber of the dorsal duct had to be greater than (that of) the ventral duct," he said.
ERP diagnosed pancreas divisum in 9/41 (21%) of patients. Compared with this standard, MDCT’s sensitivity was 100%/89%, specificity was 100%/97%, the positive predictive value was 100%/89%, and the negative predictive value was 100%/89%, for readers 1 and 2, respectively.
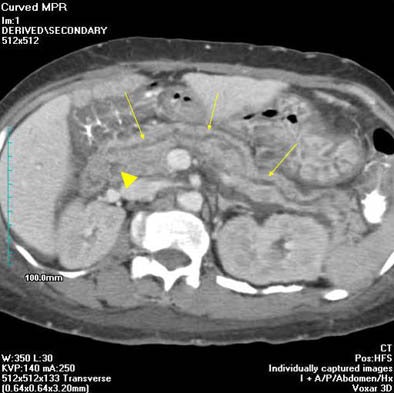 |
| Curved MPR image shows large "dominant" dorsal duct (arrows) with smaller ventral duct posteriorly (arrowhead). Images courtesy of Dr. Brian Lucey. |
"Looking at the results from the CT perspective, in five of nine patients (diagnosed with pancreas divisum), both dorsal and ventral duct were seen, where the caliber of the dorsal duct was greater than the ventral duct," he said. "In three of the patients, the dorsal duct was seen and the ventral duct was not seen. And in one patient, the pancreatic duct was not visualized by either observer -- so that was a false negative for both observers for pancreas divisum," he said.
In conclusion, carefully performed and interpreted MDCT is highly accurate for detecting pancreas divisum -- unlike what’s been reported previously for CT, Lucey said. "The main factors responsible are the fact that you’re getting a lot of thin collimated data, and the fact that using a PACS system you can actually trace these small ductal structures. And using the curved MPRs you can lay out the pancreatic duct particularly well. For these reasons we can actually see the pancreatic duct so much better, and can see pancreas divisum so much better."
By Eric BarnesAuntMinnie staff writer
April 14, 2004
Related Reading
MDCT reliably gauges vascular infiltration in pancreatic cancer, March 6, 2004
Ultrasound of the pancreas: Cystic and non-focal pathology, February 13, 2004
MR, CT detect cystic pancreatic lesions, but malignancy a tough call, February 5, 2004
Mayo group seeks to optimize pancreatic MDCT protocols, October 27, 2003
Multiphase CT shows middling sensitivity for pancreatic insulinoma tumors, October 15, 2003
Copyright © 2004 AuntMinnie.com