Unsuspected pulmonary embolism is more common than previously reported, according to researchers from Italy, who found a high prevalence of incidentally detected PE using thin-slice multidetector-row CT. Fortunately, the group also reported in a later study, preclinical probability can be a fairly reliable pretest indicator of PE risk.
Chest MDCT exams undertaken for reasons other than ruling out PE found incidental emboli in as many as 4% of hospitalized patients and 1% of outpatients, Dr. Maria Luigia Storto and colleagues wrote in the January 2005 issue of American Journal of Roentgenology. Seventy percent of the cases occurred in patients with a known thoracic malignancy, though the figure was nearly identical to the percentage of patients whose CT exam was performed for the purpose of staging a known malignancy.
An estimated 650,000 cases of PE and 50,000 associated deaths occur each year in the U.S., the group from the University of Chieti and SS Annunziata Hospital in Chieti, Italy, noted in their report. But such numbers, high as they are, probably still underestimate disease presence significantly due to the high numbers of occult PE cases, for whom treatment may well be warranted.
"A high frequency of asymptomatic pulmonary embolism has been reported in patients with deep venous thrombosis," the researchers wrote. "Silent pulmonary embolism is also reported to occur in patients with neoplastic disease, patients with hypercoagulation, and patients who have sustained trauma.... With the introduction of MDCT scanners and their high acquisition speed, thin collimations frequently are used for routine studies of the chest, which has resulted in increased spatial resolution and improved visualization of peripheral pulmonary arteries" (AJR, January 2005, Vol. 184:1, pp. 264-267).
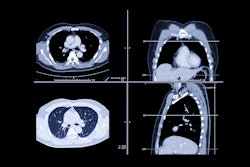
The group's retrospective study examined the prevalence of incidentally detected PE with thin-slice contrast-enhanced MDCT, and sought to determine whether the use of wide window settings might also improve detection. The group examined 589 patients (416 men and 173 women, mean age 63.4, 480 inpatients/109 outpatients) who underwent chest CT for reasons other than ruling out PE.
MDCT was performed to stage a known pulmonary neoplasm in 410 (69.6%) of the patients, and for other reasons in the remaining 179 patients, including characterization of a pulmonary nodule found on a chest film (n = 58), hemoptysis of unknown cause (n = 25), infiltrative or infectious lung disease (n = 25), pleural disease or pleural effusion, and trauma or other injury (n = 50).
Twenty-five seconds following automated injection of 80 mL of contrast material (300 mg I/mL iomeprol), images were acquired on a four-detector Volume Zoom Scanner (Siemens Medical Solutions, Erlangen, Germany) at 4 x 2.5-mm collimation, table speed of 15 mm per (0.5 second) rotation, 140 kVp and 120 mAs, and reconstruction of 5-mm-thick axial slices, the authors wrote.
Two experience chest radiologists blinded to the clinical data looked for PE (a filling defect characterized by low attenuation) in the main, lobar, segmental, or subsegmental pulmonary arteries, also indicating their subjective confidence level in each diagnosis. Each dataset was examined twice, with sessions at least a week apart, once with normal window settings (width 400 H; level 40 H) and once with wide settings (width 600 H, level 100-150 H).
Finally, the researchers reviewed the radiology reports and existing medical records to determine how many of the emboli had been reported previously.
Good or satisfactory arterial opacification was seen in 581 of 589 (98.6%) patients evaluated, the authors found. Overall, PE was detected in 20/581 patients with analyzable scans (3.4%). Among hospital inpatients the prevalence was 4% (19/474) and 0.9% among outpatients.
Fourteen of the 20 patients with unsuspected PE had underlying malignancies, including bronchogenic carcinoma (n = 8), mesothelioma (n = 2), colon carcinoma (n = 2), and renal neoplasm in one patient.
Also, 18/20 patients with PE were identified using standard window settings, but the use of wider window settings in a subsequent session enabled the identification of two additional patients with PE.
Without the use of wide window settings, the detection rate would have dropped to 3% rather than 4%, and the use of standard window settings may have contributed to the 30% rate of missed PE on the original radiology reports, the group wrote.
The group suspected that "satisfaction of search" limitations may have had a hand as well: two of the patients with missed PE on the original report had lung cancer, one had a colorectal cancer metastasis, two had pleural effusion, and one had pulmonary sarcoidosis.
"The prevalence of malignancy among patients with unsuspected pulmonary embolism was significantly higher than the prevalence of benign disease (64.7% versus 35.3%, respectively; 0.05)" the authors reported. "Even though the percentage of patients with malignancy in our study was smaller than that reported by Gosselin et al, we found a higher prevalence of unsuspected pulmonary embolism. This result may be attributable to the different CT technique and increased spatial resolution of our scanning protocol."
Finally, a review of the original radiology reports showed that 70% of the emboli had been noted in the original radiology report. Occult PE may have serious health and patient-management implications, particularly in patients with underlying cardiovascular disease, the authors noted.
"In an autopsy study, the diagnosis was unsuspected in 14 (70%) of 20 patients who died from pulmonary embolism," they wrote. "Although in a selected series of patients without severe cardiovascular disease silent pulmonary embolism had a good prognosis and the anticoagulant treatment did not influence the resolution rate of pulmonary embolism, most authors believe that occult pulmonary emboli may be the antecedent of more serious and clinically obvious emboli and may need to be treated."
Another study found a 1% rate of unsuspected PE in patients with neoplastic disease, hypercoagulation, and trauma, all conditions for which patients are routinely imaged, Storto and colleagues added.
But inasmuch as occult PE was seen in so many in the study who were inpatients with a known malignancy, the authors recommended careful evaluation of the CT images in such high-risk patients. "We also recommend the use of wide window settings for the interpretation of routine MDCT images to improve detection of unsuspected pulmonary emboli," they wrote.
CT correlates with pretest clinical probability
At the 2004 RSNA meeting in Chicago, the group presented a second PE study that concluded that the prevalence and anatomic distribution of pulmonary emboli at MDCT are strongly correlated with pretest clinical probability.
This time Storto and colleagues relied on British Thoracic Society criteria to stratify 162 patients with suspected pulmonary emboli into low, intermediate, and high probability of PE based on clinical records.
MDCT results showed the overall prevalence of PE to be 35%, while the clinical probability of PE was high in 38.8% of patients, intermediate in 35.2% of patients, and low in 26% of patients, the group reported in an accompanying abstract.
Using the same four-detector scanner and slice thickness, MDCT found PE in 72.4% of patients with high probability (65.8% involved either a main or a lobar artery), 65.5% of patients with intermediate probability (60.3% in a main or lobar vessels), and 48.2% of patient with low probability (all in segmental or subsegmental arteries), they reported.
MDCT found emboli in 72.4% of patients with high clinical probability (65.8% involving either a main or a lobar artery), 65.5% of patients with intermediate probability (60.3% in a main or lobar vessel), and 48.2% of patients with low probability (all in segmental or subsegmental arteries). The differences in distribution of thrombi between patients with high and low probability were significant (p < 0.05), but emboli were still seen in nearly half of those at low clinical risk, the group concluded.
Risk factors in Ireland
Earlier this year, a study from Ireland examined PE risk factors among 60 patients with pulmonary embolism confirmed at CT. The principal risk factors for pulmonary embolism were elective surgery (27%), medical illness (20%), primary immobility (13%), and isolated distal lower limb fracture (7%), the group wrote in the Irish Journal of Medical Science (April-June 2004, Vol. 173:2, pp. 85-88).
Some 43% of the patients had been hospitalized within the six weeks prior to PE onset, they wrote in an abstract. And some patients had undergone "low-risk" procedures without prophylaxis, but had other significant thromboembolic risk factors indicating a need for prophylaxis.
By Eric Barnes
AuntMinnie.com staff writer
December 30, 2004
Related Reading
Biosite gets FDA clearance for pulmonary embolism diagnostic test, December 6, 2004
CT imaging alone may be suitable for work-up of pulmonary embolism, November 22, 2004
Thoracic CT expert takes on chronic PE diagnosis, October 15, 2004
CT for PE: Best test gets better, September 10, 2004
MDCT drives important changes in U.K. healthcare, August 10, 2004
Copyright © 2004 AuntMinnie.com