European radiologists, like their U.S. counterparts, have embarked on new efforts to answer the very long-term question of whether CT lung cancer screening and intervention in smokers can reduce mortality.
Increasingly they are pinning their hopes on randomized prospective trials, which some experts see as the only way to reliably assess any mortality benefit associated with the CT screening of current and former smokers. Unfortunately, such trials require a control group that does not get screened for lung cancer.
Studies under way on the continent include the GranDespican trial in France, which seeks to examine 21,000 smokers and former smokers, and the Nelson trial in the Netherlands and Belgium, which aims to recruit 24,000 smokers and former smokers and follow them for years, as well as an unscreened control population of roughly equal size.
At the 2005 European Congress of Radiology (ECR) in Vienna, Dong Ming Xu from the University Medical Center Groningen in the Netherlands presented the preliminary results from the first 2,133 subjects screened by MDCT in the Nelson trial. So far more than 16,000 volunteers have been recruited, she said.
The Groningen team, led by Dr. Rob van Klaveren, includes Dr. Rozemarijn Vliegenhart. The research group also includes Dr. Matthijs Oudkerk and Dr. Harry de Koning from the Erasmus Medical Center in Rotterdam.
Together they are examining male smokers and former smokers age 50-75 with at least 20 pack-years under their belts. The volunteers were recruited, then randomized to receive screening or no screening in one of four participating centers in the Netherlands. A fifth site, in Leuven, Belgium, is also participating in the trial.
Sixteen-row CT scanners and LungCare CAD workstations (Siemens Medical Solutions, Erlangen, Germany) were used to screen the subjects, with the results determined by consensus of two radiologists, and adjudicated by a third radiologist in case of disagreement.
"All of the final results are independent of nodule enhancement during software analysis," Xu noted. "The nodules will be divided into three types: solid nodules, partly solid nodules, and the nonsolid nodules. For the solid lesions, volume will be measured automatically by the software. For the partly solid or nonsolid lesions, the diameter will be measured manually. For the solid nodules, if the volume is over 500 mm3 in three months, or the volume growth is over 25%, we consider it a potentially malignant nodule, so the volunteer will be referred to the pulmonologists for further investigation."
When patients are referred to them, the pulmonolgists order a diagnostic CT scan, PET, and perhaps a biopsy, at their discretion, Xu explained. In all, 2,133 participants underwent baseline scans between April 2004 and February 2005, and were included in the calculations.
Of these, approximately 19% had no significant pulmonary nodules, while 11% had significant and potentially malignant nodules, she said. Just 1.8% were referred to the pulmonologists for further evaluation.
"Around 11% of the test results are positive, and 1/55 pulmonary lesions were very suspicious of lung cancer," Xu said. "In the end, 1/190 (0.5%) volunteers were confirmed with lung cancer."
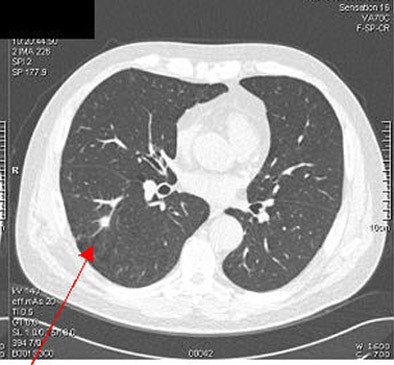
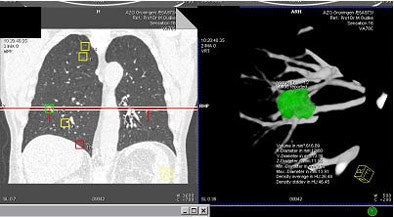 |
| Above and below: a solid nodule measuring 617 mm3, was confirmed as lung cancer. Images courtesy of Dr. Rozemarijn Vliegenhart. |
 |
The rate of probable lung carcinoma was lower than that seen in the nonrandomized International Early Lung Cancer Action Program (I-ELCAP), or the randomized National Lung Screening Trial, she said. As for other differences, "in the I-ELCAP study, approximately 60% of lung cancers were subsolid lesions, but in our study almost 100% of the lung cancers (were) solid lesions. And this finding is consistent with other literature," Xu said.
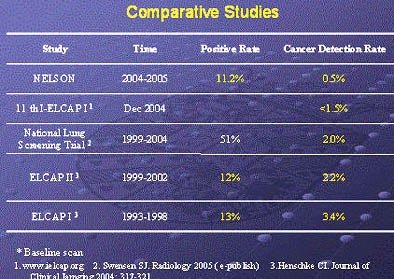 |
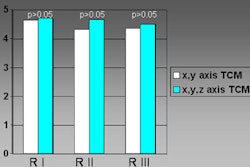
| The Nelson researchers have found fewer cases of lung cancer in their all-male cohort compared to previous screening trials. Chart courtesy of Dr. Rozemarijn Vliegenhart. |
Recruiting efforts were also conducted differently. The I-ELCAP team relied on newspaper and television ads to get the message out, and communicated with general practitioners, while the Nelson group relied exclusively on letters mailed to the general population. Lesion measurement differed as well, she said. The Nelson group calculated nodule volume using a 3D method, while the National Lung Screening Trial and I-ELCAP relied on 2D measurements, she said.
"Seven (research groups) have stated that subsolid lesions are quite common in the U.S. and Japan compared to Europe," Xu noted. "And gender is a very important factor because in the National Lung Screening Trial and I-ELCAP studies, approximately 50% of participants were women, but in our study 100% of volunteers were men."
I-ELCAP showed that women have an increased risk of lung cancer compared to men of the same age, she said. "And if a woman has a smoking history, she is twice as likely as a man to develop lung cancer." Women may be added to the Nelson trial as it progresses, Vliegenthart wrote in an e-mail message to AuntMinnie.com.
By Eric Barnes
AuntMinnie.com staff writer
April 18, 2005
Related Reading
CT screening detects early lung cancers, but mortality benefits unclear, March 17, 2005
Lung cancer screening spots lesions early, gives patients additional longevity, December 6, 2004
Diagnostic work-up of CT-detected lung cancer variable, November 22, 2004
Smaller stage I non-small cell lung cancers more curable than larger tumors, September 20, 2004
Copyright © 2005 AuntMinnie.com