As athletes become stronger and faster and their activities more intense and hard-hitting, healthcare providers are researching better methods to detect the immediate presence and long term-effects of concussions.
The University of Pittsburgh Department of Neurological Surgery estimates that more than 300,000 sports-related concussions occur each year in the U.S., while the chance of an athlete suffering a concussion while playing a contact sport could be as great as 19% per year of play.
But many concussions are not reported. When an athlete is hit in the head, feels dizzy for a few moments, and later seems to be back to normal, he or she likely will not seek medical treatment. It often takes an athlete becoming disoriented or losing consciousness before he or she is taken to an emergency room for a CT or MRI scan.
"Subtle traumatic brain injury and postconcussion syndrome are almost like silent epidemics," said Dr. Vivek Sehgal, director of MRI at Harper University Hospital in Detroit. "Even if the imaging is normal, patients can be devastated."
When an athlete arrives at the emergency room, time is critical so a five-minute CT scan is the modality of choice. "In acute settings, CT is the most common imaging modality for the simple reason that it can pick up blood," noted Dr. John Knightly, co-director of the mild trauma brain injury program at the Atlantic Neuroscience Institute, based at Overlook Hospital in Summit, NJ.
CT can quickly rule out life-threatening conditions, such as a subdural or epidermal hematoma and intracervical hemorrhages. If time and circumstances allow, a 20- to 25-minute MRI may be performed as a follow-up for prognosis, making MRI and CT complementary modalities in head trauma cases.
Imaging advances
Both 3-tesla MRI and multislice CT have enhanced physicians' ability to diagnose head trauma. "With the advent of more advanced imaging technology, we have a better view of the anatomical sequela of subacute and chronic brain injury," said Dr. Neil Horner, chief of neuroradiology at the Atlantic Neuroscience Institute. "Previously, the entities we could best image in brain injuries were the acute findings, such as fracture and acute hemorrhage. With the advent of more sophisticated MRI sequences, we are beginning to evaluate in detail the subacute and chronic phases of brain injury."
In the 1990s, conventional MRI added considerable information concerning white-matter injury, such as diffuse axonal injury (DAI). "Now newer techniques have arisen," Horner added, "allowing us to further evaluate white-matter tracks of the brain in patients who have had traumatic brain injury."
"Previously, we could look at fractures and areas of acute blood or bruising of the brain and, until recently, the late sequela or subacute or chronic sequela would be relegated to things such as atrophy related to brain injury, leaks of fluids from infarctions, or strokes related to trauma," he said.
The institute currently is evaluating an MRI technique called diffusion tensor imaging (DTI) on its 3-tesla MRI system. DTI allows physicians to view white-matter tracks -- which Horner describes as the "fiber-optic cable of the brain," providing a "communication network from one area of the brain to another" -- in greater detail and sensitivity, thus uncovering more areas of damage than conventional MRI.
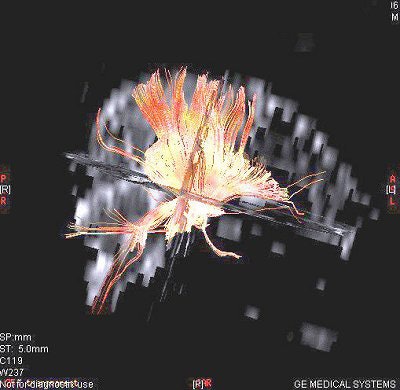 |
| The tractography 3D image is taken using diffusion tensor imaging with a 3-tesla MRI system. Image courtesy of the Atlantic Neuroscience Institute. |
DTI also can be used to view any restricted water flow in different planes or in different directions. The images can be color-coded to determine if there is an obstruction of the white-matter track. "If the white-matter tracks are damaged or their normal anatomy is disrupted, we will see the disruption of the water flow in that direction," Horner said.
Long-term prognosis
MRI is most valuable several weeks after an injury, when a CT scan looks normal, but the patient continues to exhibit signs of postconcussion syndrome and the clinician is searching for more subtle abnormalities, particularly in the area of the lower brain stem near the cerebellum. "A CT scan is not as good there because it is surrounded by bone and bone leaves artifacts. MR is a better imaging choice," Knightly said. "If we are talking about anything larger than 2 mm, CT will pick it up."
In cases of multiple concussions over time, MRI also may provide evidence of subdural hematomas or an anatomic defect that CT does not detect. "For patients with multiple concussions, it is more the history that is important and the interim between the different concussions than it is the number (of concussions)," Knightly added.
For the past year, Harper University Hospital has been developing an MRI technique it calls susceptibility weighted imaging (SWI). Under the direction of Dr. E. Mark Haacke, director of Wayne State University's MR Research Facility in Detroit, SWI is designed to detect microbleeds, vascular identifiers for petechial hemorrhages, and other conditions that CT and conventional MRI may miss.
Sehgal said early indications are that clinicians can uncover five to six times more trauma because of the sequencing technique. Harper is applying to the National Institutes of Health (NIH) for a multiproject grant on behalf of Wayne State and Loma Linda University in Loma Linda, CA.
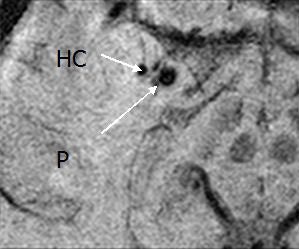 |
| Above and below, susceptibility weighted imaging technique shows bleeding in the hippocampus (HC) and the adjacent putamen (P) and globus pallidus (GP), suggesting why the patient had short-term memory loss. Images courtesy of the department of radiology at Wayne State University. |
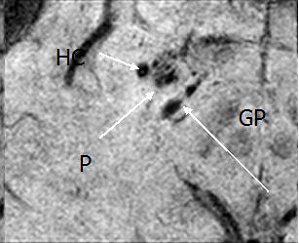 |
"We are putting together different MR sequences and techniques to evaluate subtle trauma brain injury," Sehgal said. "CT can see severe traumatic brain injury, but people with mild trauma brain injury may be told their images are normal, so that's what we are trying to find."
Sehgal noted that MR spectroscopy is a good tool for long-term prognoses in head trauma cases, adding that results appear better with 3-tesla systems. "However, there is no statistical data to prove it one way or another," he said. "When you have 3T, strength exponentially increases, but artifacts increase as well."
Neuroimaging research
Functional MRI (fMRI) also is showing potential as both a diagnostic and research tool in the assessment of concussion. A study from Florida Atlantic University in Boca Raton found that physiologic markers can be detected within days of a football player suffering a concussion, demonstrating the ability of fMRI to track a patient's progress and identify pathways to recovery (American Journal of Neuroradiology, May 2004, Vol. 25:5, pp. 738-745).
The researchers noted that with fMRI's ability to provide "task-specific information about neural function, it is well-suited to detect functional abnormalities associated with concussion."
Neural activity was evaluated by measuring changes in local blood oxygen level-dependent (BOLD) activity with a 1.5-tesla MRI system. Twenty 5-mm-thick axial sections spaced 2.5 mm apart provided coverage of the entire brain. Eight players were evaluated before the season started, and four players who suffered concussions were given the same functional tasks again within one week of the injury.
The preliminary results found "considerably greater" increases in BOLD signal intensity in football players who suffered concussions. Such increases, it is believed, reflect the brain's need for "additional neural resources" to process moderate tasks and the aftereffects of the head trauma.
MRI's worth
MRI's worth also was evident in a study by researchers at Comenius University in Bratislava, Slovakia. The team reviewed 30 patients with mild traumatic brain injury (MTBI) between January 2004 and June 2005. The patients received a neurological exam, as well as neuropsychological testing, which included a postconcussion symptoms scale questionnaire and brain scan with 1.5-tesla MRI.
MRI showed evidence of traumatic and nonspecific pathological conditions in nine patients, with traumatic lesions in seven patients. Nonspecific white-matter lesions were found in five healthy control patients.
The researchers also found "statistically significant neuropsychological differences" between MTBI patients with "true traumatic lesions and MTBI patients with nonspecific lesions." They concluded that "some acute MTBI signs and symptoms have a real organic basis, which can be detected by selected new MRI modalities" (Neuroradiology, September 2006, Vol. 48:9, pp. 661-669).
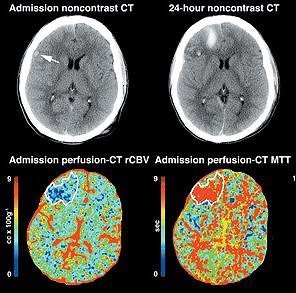 |
| Perfusion CT depicts the full extent of cerebral contusions earlier and more accurately than conventional unenhanced cerebral CT. Scans were obtained in a 20-year-old man involved in a high-speed traffic accident. At admission, unenhanced cerebral CT depicts only a small hemorrhagic focus in the right frontal operculum (arrow); however, admission perfusion CT shows a more extensive brain perfusion abnormality, involving most of the right frontal lobe (white contour). This area is characterized by low regional cerebral blood volume (rCBV), high mean transit time (MTT), and low regional cerebral blood flow (rCBF) values. Unenhanced cerebral CT scan obtained 24 hours after admission shows a hemorrhagic contusion in the exact zone that appeared to be abnormal on the admission perfusion CT scan. |
A group from the University of Rochester Medical Center (URMC) in Rochester, NY, tested MRI and CT with a review of neurologic injury in patients who suffered a concussion, focusing on patients with normal CT brain scans. The researchers also considered brain tissue pathology, CT and MRI scans, serum biomarkers, formal cognitive and balance tests, fMRI, PET, and SPECT.
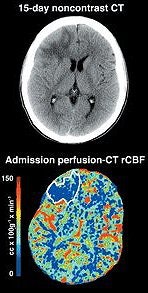 |
| Same patient as above. Abnormal zone progressed into a sequellar lesion, as evidenced by the unenhanced CT scan obtained at day 15. Figure 5. Wintermark M, van Melle G, Schnyder P, Revelly JP, et al, "Admission Perfusion CT: Prognostic Value in Patients with Severe Head Trauma," Radiology. 2004;232:211-220. |
They noted that MRI "detects more traumatic abnormalities than CT scan, but there have been few studies that focused on concussion." MRI also detected abnormalities, such as small cortical contusions or subdural hematomas, and occasionally small white-matter hemorrhages associated with axonal injury.
The most significant of the URMC group's findings is that "after concussion, a normal CT scan does not rule out the presence of brain injury," they wrote (Academic Emergency Medicine, February 2006, Vol. 13:2, pp. 199-214).
"The widespread use of the CT scan as the only diagnostic tool for head injury appears to have reduced the clinical relevance of concussion to detecting surgically correctable hemorrhage," the authors stated.
By Wayne Forrest
AuntMinnie.com staff writer
April 18, 2007
Related Readings
Brain stem lesion on MRI bodes ill for comatose head trauma patients, April 27, 2006
MRI finds long-term concussion effects, August 29, 2004
Brain damage in boxers occurs long before symptoms, November 15, 2002
Imaging is rarely definitive in concussion, February 21, 2002
Diffusion-weighted MRI useful in evaluating pediatric head trauma, October 3, 2001
Copyright © 2007 AuntMinnie.com