
In part because cancer is so rare among the smallest colorectal polyps, a new study of 100,000 hypothetical screening patients found that virtual colonoscopy is the cheapest and safest way to reduce colon cancer mortality in individuals 50 years and older.
In fact, using a minimum 6-mm polyp size threshold, VC was more than twice as cost-effective as optical colonoscopy per life year gained, researchers reported in the June edition of Cancer, which was released online before print (April 23, 2007). Even without a size threshold, the study found that virtual colonoscopy was marginally cheaper than other screening alternatives, which included colonoscopy and flexible sigmoidoscopy.
Still, the 6-mm size threshold is a valid cutoff point because the natural history of diminutive polyps argues against spending money to follow or remove them, the authors wrote. Previous cost models that provide for removal of even the smallest polyps have found the cost of screening with VC to be prohibitive.
"In general, diminutive colorectal polyps appear to cause an unjustified cost burden and high complication rate for CRC (colorectal cancer) screening," wrote lead author Dr. Perry Pickhardt, associate professor of radiology at the University of Wisconsin in Madison.
Numerous screening models have shown that "a variety of screening strategies can be cost-effective due to the prolonged, detectable preclinical phase that allows for cancer prevention," noted Pickhardt and his research colleagues Dr. Cesare Hassan and Dr. Angelo Zullo from Nuovo Regina Margherita Hospital in Rome, Dr. Andrea Laghi from the University of Rome, and Dr. David Kim, also from the University of Wisconsin at Madison. "Because of the wide variability in the available resources, patient preferences, and program adherence, a singular solution to CRC screening is unlikely to succeed."
VC's accuracy and favorable cost profile qualify it to be added to the list of reimbursed exams in the U.S., which now includes optical colonoscopy, fecal occult blood testing, and flexible sigmoidoscopy, the group explained.
The researchers developed a mathematical Markov model and applied it to a screening cohort of 100,000 hypothetical individuals of screening age at average risk for colorectal cancer, based on U.S. population data.
"The age-dependent incidence of CRC computed by the model closely simulates the National Cancer Institute's Surveillance, Epidemiology, and End Results (SEER) registry data applied to average-risk adults," they noted.
The model was designed to simulate the progression from no lesions to death from colon cancer throughout various stages of disease, including the statistical possibility of dying from a very small colorectal lesion, the authors stated.
Corresponding to the SEER data, patients are screened for CRC every 10 years from ages 50-80, while those with adenomas at baseline follow a surveillance protocol with VC at predetermined intervals. In the model as in life, some patients forego screening for their entire lives, while others drop out. Seventy-five percent of the cohort was assumed to be at average risk for colorectal cancer.
The model measured the clinical efficacy of a screening test by the reduction in CRC incidence it produced compared to no screening. "The relative cost-effectiveness of a screening test was assessed based on the additional costs required to gain an additional life year in comparison with either no screening or another screening strategy," the authors explained.
Sensitivity was "broadly varied among plausible ranges to compensate for the lack of precise knowledge in either the natural history of colorectal polyps or the performance characteristics of the various screening tests," they wrote. To ensure conservative projections, VC sensitivity assumptions were based on published meta-analyses rather than the superior results of current VC techniques.
Compared to no screening, the model predicted a reduction in colorectal cancer incidence of 31.4% for flexible sigmoidoscopy, 40.4% for optical colonoscopy, and 37.8% for virtual colonoscopy without a polyp size threshold.
The costs per life year gained were $4,361 for VC with a 6-mm reporting threshold, $7,138 for VC with no threshold, $7,417 for flexible sigmoidoscopy, and $9,180 for conventional (or optical) colonoscopy.
VC screening without reporting of diminutive lesions was considerably less expensive than primary optical colonoscopy, which soared to $63,900 per life year gained. And the incremental cost of reporting lesions 6 mm and smaller was $118,440, but that expenditure reduced the incidence of colorectal cancer by only 1.3% (from 37.8% to 36.5%).
Conversely, performing VC rather than conventional colonoscopy reduced the number of invasive endoscopic procedures by 77.6% (39,374 compared to 175,911), which reduced the number of complications of bleeding and perforation related to optical colonoscopy by 1,112.
"Given the low overall participation in CRC screening, driven in part by limited access and capacity with some tests, as well as by differences in patient preferences, a multipronged approach is likely needed to address the disturbingly high incidence of (colorectal cancer)," Pickhardt and colleagues wrote.
The authors noted that the efficacy of all screening tests modeled were highly sensitive to the input values. For example, colorectal cancer prevention drops rapidly for VC if the sensitivity for polyps 6 mm and larger drops below baseline assumptions. On the other hand, cancer prevention rises rapidly if state-of-the-art VC techniques are used rather than the older meta-analyses the authors employed in their study.
Previous models that have found higher costs related to CT colonography (CTC or VC) were based on colonoscopic removal of all detected polyps, regardless of size, the researchers added.
"It is widely accepted that polypectomy is indicated for large polyps (≥ 10 mm) detected at the time of CTC screening because the relatively small risks of undergoing therapeutic OC (optical colonoscopy) are likely outweighed by the malignant potential of these lesions," the team wrote. "Similarly, there also appears to be a general agreement that diminutive lesions (measuring ≤ 5 mm) are of no practical clinical significance because only a fraction are neoplastic, and, of these < 1% are histologically advanced and essentially none are malignant."
 |
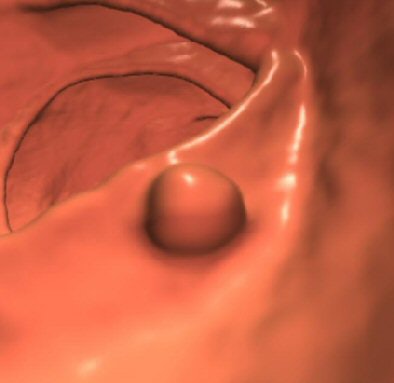
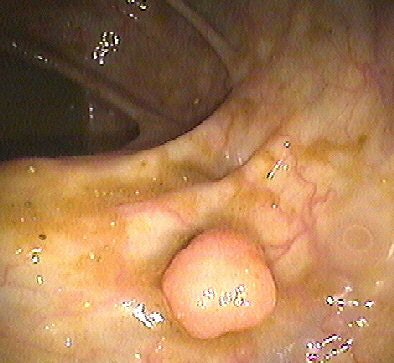
| Top, colon map from screening CTC shows the location of three polyps that measured 6-9 mm in size (C-RADS 3 classification). Below, 3D endoluminal CTC image shows a 6-mm polyp in the ascending colon. Bottom, image from same-day optical colonoscopy shows the same polyp, which proved to be a tubular adenoma. The other two polyps (8 and 9 mm in size) also proved to be tubular adenomas. All images courtesy of Dr. Perry Pickhardt. |
 |
 |
In any case, VC's sensitivity is low for the smallest lesions, they noted. And even when detected at VC, such lesions cannot always be seen on follow-up colonoscopy. Overall, "the potential benefit from OC polypectomy for a CTC-detected diminutive polyp is very likely outweighed by procedural costs and risks of the invasive procedure," the authors stated.
In addition, because the actual dollar costs of the exams are likely to vary widely over time, the general trends are more important than the actual dollar figures calculated.
"In fact, the charges/costs related to (optical colonoscopy) in our experience are three to four times greater than the charge/cost for CTC, which would have vastly affected our results and further separated their relative cost-effectiveness if included in the model," the authors wrote.
Still, VC should not be considered a replacement for optical colonography, inasmuch as the effectiveness of the population screening model depends on the "summed participation of all the individual screening options," they noted.
More controversial than the disposition of small and large polyps is the question of what to do with so-called medium-sized lesions ranging from 7-9 mm in diameter. Based on available natural history data, it could be argued that short-term VC surveillance of these lesions is a reasonable strategy. However, due to a lack of third-party reimbursement, few centers offer such surveillance, so the economic and clinical impact is uncertain. The management of medium-sized lesions (6-9 mm) will be addressed in a future study, Pickhardt told AuntMinnie.com.
"CTC with nonreporting of diminutive lesions was found to be the most cost-effective and safest screening option evaluated," the researchers concluded. "These results provide further support for the practice of a 6-mm polyp size reporting threshold at CTC screening," especially considering that removal of smaller lesions appears to add unjustified costs and clinical risks to screening.
The use of primary VC screening as a selective filter for optical colonoscopy polypectomy for lesions 6 mm and larger "represents a powerful new approach to (colorectal cancer) screening," they wrote.
Ann Zauber, Ph.D., an associate attending biostatistician at Memorial Sloan-Kettering Cancer Center in New York City, commented on the study in an e-mail to AuntMinnie.com.
"Dr. Pickhardt has addressed an exceedingly important question on the importance of removing diminutive lesions detected on CTC," Zauber wrote. "The Cancer Intervention and Surveillance Modeling Network (CISNET) of the NCI encourages collaboration in comparing microsimulation modeling assumptions and results. Such a comparison for this question would be useful and allow for a wider understanding of the implications of this approach."
By Eric Barnes
AuntMinnie.com staff writer
April 24, 2007
Related Reading
Higher costs seen in post-VC extracolonic follow-up, November 3, 2006
Extracolonic lesions: Find them if you can, October 30, 2006
Extracolonic findings double VC costs, but might be worth paying, July 20, 2006
Colorectal cancer screening could add billions to annual healthcare expenditures, November 9, 2005
VC would raise screening costs, study concludes, October 31, 2005
Copyright © 2007 AuntMinnie.com




















