Addressing the important question of myocardial viability after reperfusion therapy, higher contrast-to-noise ratios (CNRs) gave cardiac MRI an edge over 64-slice CT, according to a new study in Radiology.
Knowledge about myocardial perfusion and transmural infarct size after myocardial infarction (MI) has prognostic value as well as therapeutic consequences, explained Dr. Koen Nieman, Ph.D.; Dr. Michael Shapiro; and colleagues from Massachusetts General Hospital and Harvard Medical School in Boston (Radiology, April 2008, Vol. 247:1, pp. 49-56).
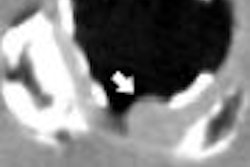
Imaging depicts these processes in two important ways: first, in the relative hypoenhancement of damaged myocardium at first-pass imaging, representing reduced microvascular perfusion of the affected tissues; and second, myocardial necrosis is revealed in the delayed hyperenhancement of affected regions -- where MRI showed superiority compared to MDCT, the authors noted.
MRI has proven value in assessing both myocardial perfusion and transmural infarct size. SPECT, which is well supported for quantification of infarct size, is limited by its modest spatial resolution. Meanwhile, expanding use of coronary MDCT "has sparked renewed interest in nonangiographic CT applications, which include imaging of MI," the authors wrote. "With multidetector CT, different patterns of myocardial enhancement, early and late after contrast material administration, have been demonstrated … in humans after acute MI in a manner comparable to that of MR imaging."
The study sought to compare 64-slice CT and cardiac MRI for assessing myocardial enhancement and infarct size early after acute reperfused MI.
Nieman and his colleagues examined 21 patients (18 men, three women; mean age 60 ± 13 years) using a 64-slice CT scanner (Sensation 64, Siemens Healthcare, Malvern, PA) within five days of first reperfused MRI (Signa Twin-Speed Excite, GE Healthcare, Chalfont St. Giles, U.K.).
They acquired electrocardiogram-gated CT images using 32 x 0.6-mm detector collimation, 120 kVp, and 850-930 mAs (radiation dose 11.8 mSv ± 3.4) following intravenous administration of metoprolol as a beta-blocker and injection of 20 mL of iodinated contrast (Visipaque, GE Healthcare) followed by a 40-mL saline flush. In 15 patients, a second, delayed-enhancement CT scan was performed seven minutes after contrast injection using a reduced tube output (100 kVp, 800 mAs) and wider 1.2-mm collimation. Short-axis 8-mm images were reconstructed throughout the cardiac cycle for both protocols.
First-pass cardiac MRI was performed on a 1.5-tesla scanner equipped with an eight-element phased-array coil and high-speed gradients. After a bolus injection of 0.1 mmol/kg gadopentate dimeglumine (Magnevist, Bayer Schering Pharma, Berlin) followed by 20 mL of saline, images were acquired over 30 phases using a hybrid gradient-echo echo-planar imaging pulse sequence. Short-axis sections were acquired every other heartbeat (repetition time/echo time 6.7/1.4 msec, flip angle 20°, 128 x 128 matrix, 34 x 34-cm field-of-view, 8-mm section thickness).
A second set of delayed-enhancement MR images was obtained 10 minutes after the administration of a second contrast bolus (0.2 mmol/kg); consecutive 8-mm thick short-axis images were acquired using an inversion-recovery prepared fast-gradient echo-pulse sequence. Proper selection of inversion time was used to optimally distinguish the dark normal myocardium from the bright delayed-enhancement myocardium.
Early hypoenhancement was seen in all MDCT and MR images -- with similar contrast levels, the results showed. First-pass CT images revealed sufficient signal intensity contrast between infarcted and remote myocardium (55.3%) and between infarcted myocardium and the left ventricular cavity (87.1%), and the respective signal intensity differences were similar for first-pass MR images (47.1% and 67.3%). Still, the CNR for differentiating hypoenhanced from normal myocardium was better for first-pass MR versus first-pass CT images (p < 0.001).
Despite good correlation between the two modalities (R² = 0.72), first-pass CT showed a significantly larger perfusion defect (mean difference 4% ± 3, p < 0.001) compared to first-pass MRI. MRI's CNR advantage was even greater in delayed hyperenhancement, which was seen in 11 of 15 CT exams, compared to all 15 cardiac MRI scans. However, three of the CT studies were deemed inaccessible, owing to image noise (n = 2) and streak artifacts (n = 1).
The most important difference between the modalities, by far, was in the signal intensity between hyperenhanced and remote myocardium, which was significantly higher for delayed-enhancement MRI (272.7%) than for delayed-enhancement CT (29.3%) (p < 0.001). The difference in signal intensity between hypoenhanced and remote myocardium was 23.6% at MRI versus 36.9% at delayed-enhancement CT.
In addition, hypoenhanced areas as a percentage of left ventricular mass were well correlated between delayed-enhancement CT (13% ± 9) and cardiac MRI (15% ± 4, R² = 0.55), the researchers wrote. Delayed hypoenhancement was well correlated between the modalities (R² = 0.85%).
While studies have shown conflicting results regarding the overestimation of infarct size at CT, the study was the first the authors were aware of to quantify late hypoenhancement, which showed excellent correlation between the two modalities, they explained.
"In our study we found that early hypoattenuation can be clearly differentiated from normal myocardium," Nieman and colleagues wrote. "Given the good attenuation difference between infarcted and normal myocardium, the lower CNR at first-pass CT may in part be the result of higher spatial resolution of CT. Without the ability to null the signal from remote myocardium, delayed imaging at CT has significantly lower CNR than MR imaging, confirming earlier observations."
Certainly, cardiac assessment doesn't begin and end in the myocardium. In addition to myocardial viability, the comprehensive use of CT can provide clinically useful information in other areas, such as assessing the patency of the culprit lesion after thrombolysis and assessing the coronary arteries and left ventricular function, potentially sidestepping the need for invasive studies, the authors noted.
"Although the amount of irreversibly injured myocardium is underestimated, early hypoenhancement is a stronger negative predictor of functional recovery than total infarct size at delayed enhancement, even when reperfusion of the epicardial vessels can be achieved," they added. "Assessment of early hypoenhancement at CT may provide sufficient information to predict functional recovery similar to nuclear imaging or echocardiography."
Imaging of delayed hyperenhancement has superior contrast at MRI, the authors concluded, citing MRI's lack of radiation as an additional benefit. In CT, the more liberal use of contrast media and other protocol adjustments may improve image contrast in future studies, they wrote.
By Eric Barnes
AuntMinnie.com staff writer
May 8, 2008
Related Reading
Contrast agent osmolality makes no difference in PCI of renal disease patients, April 17, 2008
Myocardial fibrosis tied to ventricular arrhythmias, April 11, 2008
Tissue Doppler beats standard echo in predicting heart failure, April 11, 2008
Dual-source CT edges into cardiac SPECT turf, March 6, 2008
Myocardial functional reserve reduced in hypertension and diabetes, September 7, 2006
Copyright © 2008 AuntMinnie.com