When used as a second reader by an experienced chest radiologist, chest radiography computer-aided detection (CAD) technology can yield a high level of sensitivity, specificity, and accuracy in detecting lung nodules, according to a recent study published in the Journal of Digital Imaging.
The retrospective study, led by William Moore, MD, of Stony Brook University Hospital in Stony Brook, NY, found a particular benefit in improving specificity for detecting nodules 5 to 15 mm in size (J Digit Imaging, March 31, 2010).
"If you use this device as it's intended, as a second look, something to bring your attention to an area, your specificity can be in the mid-80s [and] accuracy around high 70 [or] low 80 percentile," Moore told AuntMinnie.com. "That's pretty spectacular when you're talking about pulmonary nodules between 5-mm and 15-mm size."
The research team sought to determine the performance of a chest radiography CAD system in patients referred to chest CT angiography (CTA); CTA was used as a reference standard.
The study included 240 patients from November 2007 to November 2008 who had CT-confirmed nodules and a posteroanterior radiograph within a 24-hour time frame.
All of the chest radiographs were manually sent to a U.S. Food and Drug Administration (FDA)-cleared chest radiography CAD system, the IQQA-Chest CAD (EDDA Technology, Princeton, NJ), as a DICOM image. CTA images were generated using a LightSpeed 4 scanner (GE Healthcare, Chalfont St. Giles, U.K.).
Only nodules between 0.5 and 1.5 cm were analyzed in the study. The IQQA-Chest CAD system is designed to ignore any nodule outside of these parameters.
All imaging studies were performed from the lung apex to the lung bases. CAD findings were scored from 1 to 5:
- Definitely not a nodule
- Probably not a nodule
- Unsure
- Probably a nodule
- Definitely a nodule
The chest radiographs were exposed at 100 kV with a 10:1 grid and were obtained using a FCR 9501 computed radiography system (Fujifilm Medical Systems USA, Stamford, CT). The CTA and the chest radiographs were evaluated at different times by the same experienced thoracic radiologist to avoid bias.
 |
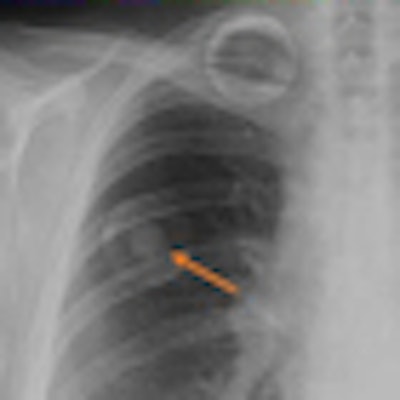
| Researchers found CAD to improve sensitivity. |
Of the 165 CAD findings or regions of interest (ROIs) on chest radiography, 49 were actual nodules seen on CTA. No definitive correlation with size of the nodule and CAD detection of the nodule was noted. There were 121 cases where there was no CAD ROI, and the CTA showed no nodules between 5 and 15 mm.
False-positive ROIs totaled 116, achieving an overall sensitivity of 71% and a specificity of 50%. The sensitivity decreased to 69% when excluding the four granulomas.
Eighty-seven of the 165 findings received a score of 1 or 2 by the radiologist and were easily dismissed. The CAD software produced 71.5% false-positive ROIs.
CTA demonstrated no nodule or other abnormality in this region. Specificity was 78% and accuracy was 74%. Five ROIs ranked as either 1 or 2 by the radiologist using CTA were determined to be true nodules.
Specificity gain
At baseline, the CAD system had moderate sensitivity of 71% and very low specificity, according to the authors. However, when used as a second reader by the experienced radiologist, specificity increased to 78% (and to 80% when easy-to-dismiss nodules were excluded).
Accuracy with the radiologist was 74%. However, five CAD ROIs determined to be true nodules by CTA were dismissed, representing 10% of all true nodules originally found by CAD.
The evolution of CAD's routine use with CT and x-ray in detecting cancerous lesions comes with a crucial caveat.
"The device performed extremely well when [used] as it's intended, and that's as a second read or an assistant to the radiologist," Moore said. "Blind use of any CAD device ... is totally inappropriate because the devices are designed to be highly sensitive, but not necessarily very specific, which is why the radiologist really needs to interact with these tools as much as possible."
The researchers acknowledged several limitations to their study. First, it did not attempt to determine a correlation between the chest radiography reports and CAD results. If all nodules seen by the CAD system were also seen by the radiologist, the system would offer little benefit.
The study notes a potential downside to the use of CAD that was not evaluated in the study. If there were no additional findings and there was an average of 0.48 false positives per case, there could be a deleterious effect on the specificity of the radiologist.
The researchers recognized CTA with 1.25-mm images as an excellent method to evaluate the lungs, but added it is not the gold standard.
They also observed that a potential population bias could have been introduced via the emergency department physician ordering trend. If the ED physicians noted a lung nodule on chest radiography, they may have been more likely to order a CTA, according to the authors.
By Lin Muschlitz
AuntMinnie.com contributing writer
June 18, 2010
Related Reading
Lung CAD performs best as second reader, May 7, 2010
Lung CAD boosts radiologist accuracy, February 17, 2010
CAD for chest x-ray detects overlooked subtle lung cancer, June 23, 2009
Computer-aided system increases detection of early-stage lung cancer, May 4, 2009
CAD provides mixed benefits for DR lung exams, March 8, 2008
Copyright © 2010 AuntMinnie.com