The turf war over uterine artery embolization (UAE) has escalated as a gynecologist goes on the offensive, suggesting that his specialty would be better suited to perform the procedure. But interventional radiologists have fired back, stating that gynecologists are simply not properly trained for such technical, imaging-based surgery.
In an article in Clinical Obstetrics and Gynecology, Dr. Bruce McLucas, from the University of California, Los Angeles, offered "a rationale and potential methodology for training and credentialing obstetrician-gynecologists in the performance of uterine fibroid embolization (UFE)" (March 2003, Vol. 46:1, pp. 70-75).
In his argument, McLucas said that ob/gyns have an advantage over interventionalists because the former are fully exposed to the pelvic vascular anatomy as part of their overall surgical training. In addition, post-procedure and follow-up should be handled by the doctor who performed the surgery, rather than the current referral system.
The transference of a procedure from one specialty to another is not new, McLucas went on to write, citing the shift of angiography from radiology to cardiology as one example. McLucas outlined a proposed UAE credentialing path for ob/gyns that included:
- Fulfillment of an educational course focusing on areas such as pelvic anatomy, radiation safety, and complications.
- Completion of 100 catheterizations, during half of which the ob/gyn will be the primary operator.
- Performance in 50 therapeutic embolizations. The ob/gyn will be the primary operator in 25 of those cases.
- Caseload amassed over a three-year period.
- A qualified interventionalist to proctor the credentialing process.
The counterpoint to McLucas came in a Journal of Vascular and Interventional Radiology commentary by Dr. James Spies from Georgetown University Medical Center in Washington, DC and Dr. David Sacks from the Reading Hospital and Medical Center in West Reading, PA. Their main argument was that the training standards put forth by McLucas were inadequate, especially for a procedure as delicate as UAE.
From a technical standpoint, UFE requires a particular understanding of the vascular anatomy that is not always covered by general surgical training, Spies and Sacks said. In addition, "UAE often requires a co-axial approach with microcatheters, which requires a much higher level of skill" (JVIR, February 2004, Vol. 15:2, pp. 111-113).
Another major issue is radiation dose. McLucas suggested radiation safety would be covered in an educational course, but Spies and Sacks said that was not enough. UFE may produce some of the highest patient radiation doses of all fluoroscopically guided interventions, even when performed by "appropriately trained operators," the interventionalists responded.
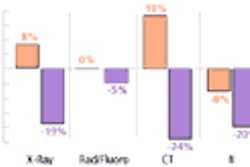
The authors went on to compare McLucas’ credential proposal with the current SIR training standards, in place since 2001:
- Complete performance of 25 UAE procedures as a primary operator.
- Successful performance in training cases.
- No significant complications for the first 100 angiographic training cases.
- No more than four cases with complication rates thereafter during training.
They stressed that the SIR standards consider a bilateral embolization as a single procedure, whereas McLucas recommended that a bilateral embolization would count as two procedures. McLucas does not mention training cases or complication rates in his standards, they wrote.
Finally, "McLucas requires that the physician needs to be the primary operator in only 25 procedures...the experience from half the procedures in McLucas’ guideline could be as an assistant," they said.
Money matters
The McLucas article may come across to some as an interesting about-face: Historically, the ob/gyn community has expressed reservations about UFE, calling for more research to back up its efficacy. As recently as January 2004, the American College of Obstetricians and Gynecologists (ACOG) issued an opinion on UFE stating that "there are insufficient data at this time to ensure that UAE is safe for women who may wish to become pregnant in the future...according to ACOG, this procedure is still considered investigational. " So why the sudden interest in performing the procedure?
"There will always be some minority (of interest) that will be finance-driven. I think there is an element of that, but people don’t really want to talk about it," said interventionalist Dr. John Lipman from Radiology Associates of Atlanta. "Clearly, that’s not the whole story, but it is a factor." Lipman and colleagues will present the results of a prospective trial comparing UAE to myomectomy tomorrow at the 2004 Society of Interventional Radiology (SIR) meeting in Phoenix.
While neither McLucas nor Spies and Sacks mention reimbursement in their pieces, no doubt it is an issue. A number of payors do cover UAE, although coverage is conditional, according to a list complied by SIR. The various CMS codes for UAE (37204, 36247X2, 75736X2, 75894, and 75898 [X2]) have a zero-day global period, indicating that services provided on the same day of the procedure are not separately reportable. It’s the interventional radiologist who is reimbursed solely for the UAE procedure whether or not they provide post-procedural care.
Another financial aspect of UAE that may appeal to payors if not gynecologists: It may prove to be more cost effective than hysterectomy, potentially depriving gynecology of one of its main revenue sources. According to an analysis by investigators at the Boston-based Institute for Technology Assessment, Massachusetts General Hospital, UAE was more effective (8.29 quality-adjusted life-years vs. 8.18) and less expensive ($6,916 vs. $7,847) than hysterectomy (Radiology, January 2004, Vol. 203:1, pp. 207-213).
"Gynecologists are used to taking care of everything having to do with (women’s health) and here’s something new that’s totally outside of their purview. In the past, gynecologists haven’t been that interested in outsourcing women’s healthcare," added Lipman, who served as one of the authors of the 2001 SIR UAE training standards.
Not a ‘drive-by’ procedure
To some degree, interventional radiology must take responsibility for the fact that gynecology has looked askance at UAE, according to Lipman. It’s not enough to offer the procedure; interventionalists must get used to providing full clinical care.
"One of the problems here is that IR, in general, has not accepted clinical responsibility for the patient. That has been a big issue with the gynecologists," he explained. "Unfortunately, there were a lot of ‘drive-by’ procedures and all the care goes back to the gynecologists. That has plagued us more than anything else. We need to step up clinically and take care of these patients."
Stepping up full patient care will be a topic of discussion at the SIR conference. On Saturday, a categorical course and a plenary session will be devoted to the latest advances in UAE, including practice management issues.
The plenary session, entitled "UAE: Late Outcomes Prove Value," will be moderated by Lipman. Speakers will include Dr. Gary Siskin from Albany Medical College in Albany, NY, who will share strategies to introduce a UAE program at a practice or institution. Siskin will then moderate the categorical course, "Lessons Learned: UAE." Spies will serve on the panel to discuss post-UAE patient communication.
Of course, the ideal situation would be for interventionalists and ob/gyns to continue working together on providing optimal UAE services. A shift in referral patterns is one sign indicating that amicable relations can be maintained between the specialties, Lipman said. When he first began performing UAE, the majority of his patients were self-referred; these days, gynecologists are sending potential candidates his way.
Without the support of their ob/gyn colleagues, interventionalists may find themselves fighting an even greater uphill battle.
"I intend to speak about my experience with building my UAE practice," Siskin wrote in an e-mail to AuntMinnie.com. "I do acknowledge the difficulties that gynecologists likely have in referring patients for this procedure, but I also believe that a gynecology buy-in to this procedure is going to be necessary for the long-term survival of the procedure. I can tell you that...we will be talking about practice development and about building relationships with gynecology."
By Shalmali PalAuntMinnie.com staff writer
March 25, 2004
Related Reading
Ob/Gyn group advises against uterine artery embolization for certain women, February 4, 2004
Uterine Fibroids: Embolization and Other Treatments, February 3, 2004
MRI shows positive post-treatment results in fibroids, leiomyomas, January 21, 2004
Cheaper UAE edges out hysterectomy for uterine fibroid treatment, January 17, 2003
Copyright © 2004 AuntMinnie.com