A minimally invasive treatment called uterine artery embolization (UAE) may be a promising alternative to hysterectomy in women due to severe bleeding after childbirth, according to experts at Michigan State University in East Lansing.
During a March 19 media briefing held by the Society of Interventional Radiology (SIR), resident Younes Jahangiri, MD, and interventional radiologist James Morrison, MD, presented a retrospective review of 66 patients (median age, 31) who underwent UAE for uncontrolled postpartum hemorrhage at their hospital between 2014 and 2022.
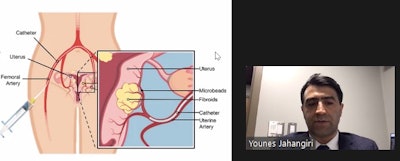 Younes Jahangiri, MD, of Michigan State University, described a procedure called uterine artery embolization at a March 19 media briefing held by the Society of Interventional Radiology.
Younes Jahangiri, MD, of Michigan State University, described a procedure called uterine artery embolization at a March 19 media briefing held by the Society of Interventional Radiology.
According to the findings, UAE successfully controlled postpartum hemorrhaging in 62 of the 66 patients (94%).
“As the medical community looks for ways to provide better care for women to address maternal health and peripartum care, [UAE] is one more option on the table that could help many women,” Jahangiri said.
Postpartum hemorrhage is a rare but potentially deadly complication of childbirth. To stop it, obstetricians first typically use conservative approaches to replace the lost blood or to promote clotting. If these measures are insufficient, however, hysterectomy is usually performed.
Alternatively, interventional radiologists can be brought in to perform UAE, the researchers explained. This procedure is performed by injecting tiny particles into the arteries that supply blood to the uterus using fluoroscopic imaging guidance. Once placed in the arteries, the particles temporarily block blood flow to stem uterine bleeding.
Four of the 66 patients in the study required hysterectomies to stop the bleeding, all of whom lost at least 2,400 ml of blood prior to presentation for UAE and who had symptoms of diffuse intravascular coagulopathy, a clotting abnormality, Jahangiri noted.
In addition, after a median duration of 20 months, five patients (8%) underwent additional intervention with hysterectomy for hemorrhage control or other reasons and 10 (16%) had successful pregnancies, although four resulted in abortion, the researchers noted.
“Based on these findings, we would encourage obstetricians to involve interventional radiologists early, to be ready to perform UAE if more conservative approaches are not managing postpartum hemorrhage,” Morrison added.
Ultimately, the researchers plan to expand their research to include multiple institutions and to conduct a prospective study that examines longer-term outcomes of UAE.
The study was presented ahead of the SIR 2024 annual meeting to be held Mar 23 to 27 in Salt Lake City, Utah.