MRI can identify risk factors in patients with subacute knee symptoms that can lead to localized knee osteoarthritis 10 years later, according to a study published online in Radiology.
Researchers at Leiden University Medical Center in Leiden, the Netherlands -- led by study co-author Kasper Huetink, MD -- also found that MRI's ability to detect those risk factors did not depend on the surgical treatment of the findings.
Osteoarthritis of the knee is a common problem, with more than 30% of the population older than 60 having detectable knee osteoarthritis, according to the researchers. MRI is beneficial in its ability to view cartilage damage, subchondral bone, and bone marrow lesions and, thus, has the potential to assess the development of osteoarthritis.
The researchers used data from an MRI study conducted 10 years ago on the effect of 0.5-tesla MRI-guided treatment on the outcomes of 855 patients with subacute knee problems.
The current study included 326 patients with a mean age of 42 years. There were 218 men and 108 women. Of the 529 excluded subjects, five patients had died, 21 patients were excluded because of MRI or radiographic contraindications, 87 patients refused participation, and 416 patients did not respond to requests to participate in the study.
Study comparisons
Findings and treatment data from the previous study were compared with follow-up radiographs and 3-tesla MRI (Achieva 3.0T, Philips Healthcare, Andover, MA) findings in the current study.
In the analysis of MR images, the researchers found that patients with anterior cruciate ligament (ACL) ruptures had an increased risk of developing joint space narrowing, cartilaginous defects, osteophytes, bone marrow lesions, and subchondral cysts medially or laterally.
In addition, patients with medial meniscal tears had an increased risk of developing joint space narrowing, cartilaginous defects, osteophytes, and bone marrow lesions medially.
As for patients with lateral meniscal tears, they exhibited an increased risk of developing joint space narrowing, cartilaginous defects, osteophytes, bone marrow lesions, and subchondral cysts laterally.
Meniscectomy, the surgical removal of all or part of a torn meniscus, had no effect on the risk of developing osteoarthritis.
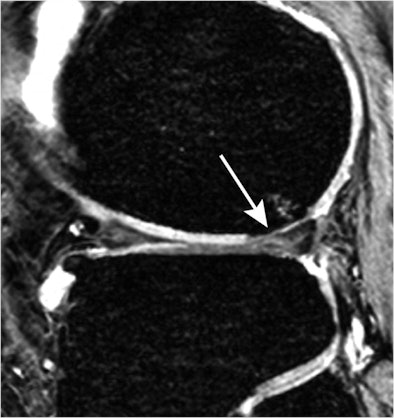 |
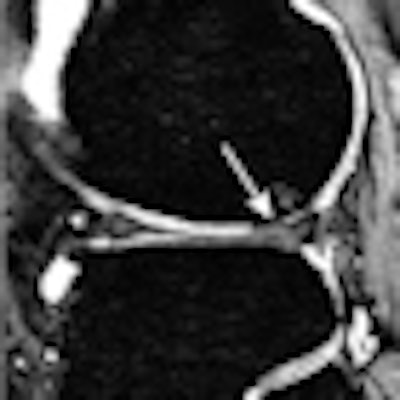
| Sagittal 3D gradient-echo MR image shows cartilaginous defect (arrow) and bone marrow lesion in lateral femoral condyle in a 54-year-old woman with ACL rupture and meniscal tears 10 years ago. The sequence was used to score the cartilage lesions. Fat-suppressed fast spin-echo sequence was used to score the bone marrow lesion. The ACL rupture was not reconstructed, and the medial meniscal tear was treated with partial meniscectomy. Image courtesy of Radiology. |
In conclusion, the authors wrote that "irrespective of treatment, the risk factors seen on knee MR images resulted in localized development of osteoarthritis 10 years later."
The different patterns of developing osteoarthritis are determined according to the initial ACL and meniscal injuries, they also noted. "The hallmark finding of osteoarthritis development after medial meniscal tears is diffuse medial cartilage loss, and after lateral meniscal tears, it is focal lateral cartilage loss. After ACL rupture, osteoarthritis characteristics are seen medially and laterally," they wrote.
By Wayne Forrest
AuntMinnie.com staff writer
June 30, 2010
Related Reading
Software saves time by segmenting meniscus in knee MR images, February 1, 2010
Sodium MRI at 3 tesla detects early signs of osteoarthritis, February 5, 2009
U.K. study finds direct access to knee MRI is cost-effective, April 3, 2008
AAOS study: MRI overused for knee osteoarthritis, March 6, 2008
Presence of osteoarthritis influences bone bruise prognosis, August 22, 2007
Copyright © 2010 AuntMinnie.com




















