Most women in the U.S. don't believe they've experienced healthcare disruptions related to the COVID-19 pandemic -- despite the documented decline in mammography screening rates, a study published September 6 in Preventive Medicine Reports found.
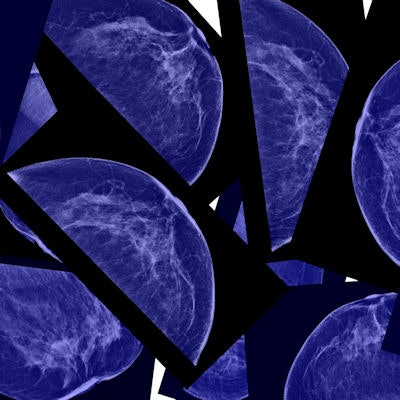
About 40% of U.S. women have received a mammogram and 12% have received screening breast MRI since the beginning of the COVID-19 pandemic, a team led by Claire Conley, PhD, from Georgetown University found. What's more, on average, women reported low levels of COVID-related healthcare disruptions.
However, the same could not be said for women who were younger and not working, a finding that suggests that factors other than the pandemic may be to blame for lower screening rates.
"Taken together, these data suggest that participants did not perceive that the COVID-19 pandemic had a significant impact on their ability to get preventive healthcare, including breast cancer screening," Conley and colleagues wrote.
Previous research has shown that the COVID-19 pandemic caused delays in preventive healthcare, including breast cancer screening, with at least one recent study finding that it cut breast screening rates in half worldwide. Experts over the past couple years have pondered whether these delays will have long-term consequences on breast cancer occurrence and mortality rates down the line.
Up to 15% of U.S. women are considered high risk for developing breast cancer. These women should have supplemental MRI scans along with annual screening mammography and alternate at six-month intervals, guidelines recommend.
Conley et al wanted to describe COVID-related healthcare disruptions and identify sociodemographic characteristics tied to these disruptions, noting a lack of data exploring the impact of COVID-19 on preventive healthcare among high-risk women. They used secondary data from a cross-sectional survey of women with greater than or equal to 20% lifetime risk of developing breast cancer.
The team examined data from a total of 225 women with an average age of 44.4 years who responded to the survey. Out of these, 203 were non-Hispanic white women.
Out of the total, 105 participants (47%) had received at least one type of breast cancer screening. More in-depth, 90 (40%) had received a mammogram and 27 (12%) had received a screening breast MRI.
Using a five-point Likert scale, the group found an average score of 1.97, indicating women "neither agreed nor disagreed" with the notion of experiencing COVID-related healthcare disruptions.
The researchers also explored factors linked to these healthcare disruptions. They found that women who were younger and not working reported significantly more COVID-related healthcare disruptions. Also, women from any other racial or ethnic group reported fewer such disruptions compared non-Hispanic white women.
They found that disruptions were most likely to be experienced by younger women, those of color, and women who were not working.
The authors suggested factors other than the pandemic may be at play for lower screening rates, noting the women's overall perception that the pandemic did not cause significant disruption.
One reason they suggested was that in the context of breast cancer screening for high-risk women, women who are younger and identify as non-Hispanic white are more likely to receive recommended screening in normal circumstances. Thus, these women are also more likely to have had that care disrupted during the pandemic, Conley and colleagues wrote.
For women who are not working, the authors wrote that women in this group consist of full-time homemakers, retirees, and students, as well as women unable to work or between jobs.
"Many of these groups may be at higher risk for complications due to COVID-19; for example, full-time homemakers may be caring for young children, retirees may be older, and individuals who are unable to work may have chronic medical conditions," they wrote. "Thus, it is possible that perceived risk of COVID-19 may have contributed to disruptions in medical care for this group."
While the researchers called for more research in these areas, they suggested that efforts to encourage high-risk U.S. women at high risk for breast cancer to return to routine preventive care may need to be targeted toward women who are younger, not working, and non-Hispanic white.




















