An automated AI model can identify incidental, extrapulmonary structures on chest CT scans and thus help clinicians predict all-cause mortality risk, researchers have reported.
A group led by Anna Marcinkiewicz, MD, PhD, of Cedars-Sinai Medical Center in Los Angeles found that the model predicted 10-year all-cause mortality with an area under the receiver operating curve (AUC) of 0.72 (p < 0.001.) The findings were published September 17 in Radiology.
"By combining imaging features from all visible structures [in our AI model], it was possible to identify participants at increased mortality risk in a large multicenter study with various CT scanners and noncontrast image acquisition protocols," the group noted. "Importantly, the model ranked the importance of each structure with respect to the risk of mortality individually for each participant."
Incidental findings on chest CT are common and can often need follow-up, the team explained. The group noted that in the National Lung Cancer Screening Trial (NLST), significant incidental findings were identified in more than a third of participants, and of these, 57% were extrapulmonary.
Marcinkiewicz and colleagues conducted a study that included 24,401 participants in the NLST who underwent low-dose CT between August 2002 and September 2007. Follow-up of these patients continued through December 2015. All-cause mortality was assessed at two-year and 10-year follow-up from baseline imaging.
Of the study cohort, 3,880 participants had 4,283 extrapulmonary findings. Of these, most were cardiovascular abnormalities (36.5%), followed by abnormalities above the diaphragm (31.9%) and below (30.9%). The researchers used TotalSegmentator (developed by Swiss researchers in 2023) to segment 32 body structures and extracted from each of these 15 radiomic features (for a total of 480 features).
| Performance of an "all-imaging" AI model for predicting all-cause mortality from chest CT data | ||
|---|---|---|
| Measure | AUC | p-value |
| 10-year all-cause mortality | 0.72 | 0.39 |
| 2-year all-cause mortality | 0.71 | 0.006 |
| Significant incidental findings | 0.7 | < 0.001 |
The investigators also reported that the model ranked the importance of each extrapulmonary structure as it related to mortality risk, an "approach [that] could assist radiologists in identifying high-risk image features that are not their primary focus," the group noted.
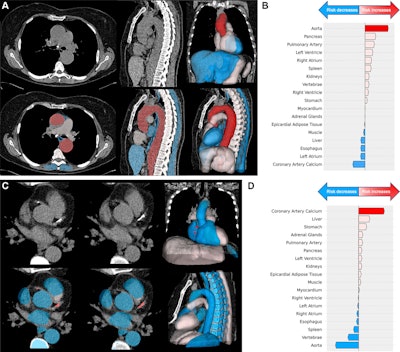 Examples of images in participants who underwent low-dose chest CT for lung cancer screening with cardiovascular structures identified at high risk of mortality, with red indicating the structure with the highest risk score, pink indicating structures with an increased risk score, and blue indicating structures with a low risk score. (A) Axial (left) and sagittal (middle) low-dose CT scans, with corresponding deep learning structure segmentation (bottom), and three-dimensional reconstructions (right) of segmented and ranked structures in a 64-year-old female participant show an aortic aneurysm (cross-sectional diameter of ascending aorta is 51 mm and descending aorta is 43 mm). (B) Waterfall plot in the same participant shows the aorta (red arrow) contributed most to death probability compared with other segmented structures. The participant died of a thoracic aortic aneurysm rupture 5 years after trial randomization. (C) Axial low-dose CT images (left, middle), with corresponding deep learning structure segmentation (bottom), and three-dimensional reconstructions (right) of segmented and ranked structures in a 62-year-old female participant show coronary artery calcifications in the right coronary artery and left descending artery. (D) Waterfall plot in the same participant shows coronary artery calcium (red arrow) contributed most to predicting mortality compared with other segmented structures. The participant died 2 years and 2 months after randomization because of acute myocardial infarction.
Examples of images in participants who underwent low-dose chest CT for lung cancer screening with cardiovascular structures identified at high risk of mortality, with red indicating the structure with the highest risk score, pink indicating structures with an increased risk score, and blue indicating structures with a low risk score. (A) Axial (left) and sagittal (middle) low-dose CT scans, with corresponding deep learning structure segmentation (bottom), and three-dimensional reconstructions (right) of segmented and ranked structures in a 64-year-old female participant show an aortic aneurysm (cross-sectional diameter of ascending aorta is 51 mm and descending aorta is 43 mm). (B) Waterfall plot in the same participant shows the aorta (red arrow) contributed most to death probability compared with other segmented structures. The participant died of a thoracic aortic aneurysm rupture 5 years after trial randomization. (C) Axial low-dose CT images (left, middle), with corresponding deep learning structure segmentation (bottom), and three-dimensional reconstructions (right) of segmented and ranked structures in a 62-year-old female participant show coronary artery calcifications in the right coronary artery and left descending artery. (D) Waterfall plot in the same participant shows coronary artery calcium (red arrow) contributed most to predicting mortality compared with other segmented structures. The participant died 2 years and 2 months after randomization because of acute myocardial infarction.
Using AI in this way with incidental chest CT findings could improve patient care, wrote Masahiro Yanagawa, MD, PhD, and Akinori Hata, MD, PhD, both of Osaka University Graduate School of Medicine in Japan in an accompanying commentary.
"The ensemble AI in the present study can comprehensively evaluate extrapulmonary lesions on chest CT scans, potentially enabling tailored personalized medicine without increasing costs or radiation exposure," Yanagawa and Hata noted.
The complete study can be found here.



















