Ignore cardiac FDG uptake in oncological PET/CT at your peril. That's the key message of new research presented at this month's European Society of Cardiovascular Radiology (ESCR) congress in Milan, which also underlined that MRI is a useful technique for evaluation of complex cases and can help to differentiate between benign and malignant lesions.
Led by Dr. Esin Gezmis, a radiologist from Izmir, Turkey, the researchers were keen to highlight the contribution of cardiovascular MRI (CMR) to further evaluate cardiac FDG uptake in oncological PET/CT imaging, which is a controversial subject because of the variability. They were not aware of any previous studies or case reports about cardiac avidity in patients with apical hypertrophic cardiomyopathy (HCM) on oncological FDG-PET/CT.
 Dr. Esin Gezmis.
Dr. Esin Gezmis.The most common metastatic sites of lung cancer are bone, brain, liver, and adrenal glands, but it can spread to nearly any organ, including the heart. Lung cancer can spread to the heart and pericardium, and metastatic involvement of the heart is approximately 40 times more prevalent than primary cardiac tumors and is generally associated with a poor prognosis, Gezmis explained. Primary lung cancer represents 36% to 39% of cardiac metastases.
"Identifying the tumor, node, and metastasis (TNM) stage of the lung cancer correctly is very important, because the determination of the appropriate treatment is mainly based on that," she stated. "The evidence of intra- and extrathoracic metastasis changes the management of these patients, and can eliminate the surgery option, which generally results in a poorer outcome."
Benefits of whole-body PET/CT
Several studies have shown the best method for lung cancer staging is FDG whole-body oncological PET/CT due to its high sensitivity and specificity, plus its ability to explore the entire body at once and reveal the metastasis. PET/CT can detect unsuspected distant metastasis in up to 30% of cases, but during routine reporting of FDG-PET/CT scans, it is common to find areas of increased FDG uptake that are unlikely to be related to the neoplasm. These findings usually require further investigation.
"The cardiac avidity in oncological FDG-PET/CT is a controversial subject, and there are conflicting studies about the importance of it and how to approach it," Gezmis said. "The main reason is that the patients undergoing this scan are studied in the fasting state, in which heart derives energy from free fatty acids (FFAs) instead of glucose, so that theoretically any cardiac avidity should be regarded as abnormal."
For clinical purposes, normal myocardial FDG activity can be defined as either absent, diffusely increased (with or without heterogeneity), focally increased (e.g., papillary muscles), or regionally increased, particularly in the posterolateral and basal parts of the heart. Enlargement of left and right ventricles because of various reasons such as hypertension, valvular disorders, and cardiomyopathies may cause diffuse FDG uptake, she continued.
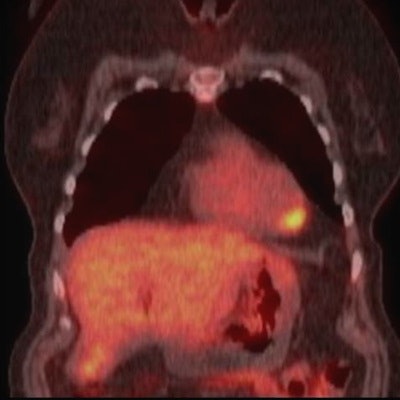
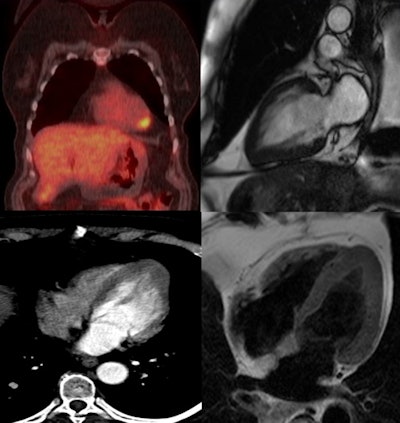 Whole-body PET/CT (top left) shows lung cancer and FDG avidity at the left ventricular apex. Image courtesy of Dr. Esin Gezmis.
Whole-body PET/CT (top left) shows lung cancer and FDG avidity at the left ventricular apex. Image courtesy of Dr. Esin Gezmis.Also resulting in cardiac FDG activity are inflammatory lesions like myocarditis, which tends to show regional uptake, and endocarditis, in which avidity at the valves is seen. Focal FDG uptake can also be observed due to cardiac involvement of sarcoidosis, particularly in the acute inflammatory stage, but it is difficult to differentiate it from cardiac neoplasms and metastasis, according to Gezmis.
In addition, lipomatous hypertrophy of interatrial septum and pericardial fat tissue might show FDG activity because of the brown fat they contain. Increased or decreased FDG uptake following a coronary artery distribution raises the possibility of coronary artery disease, although caution must be taken when making this diagnosis, as normal physiological patterns such as posterolateral avidity can mimic coronary artery disease, she added.
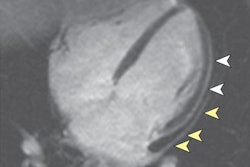
Apical HCM is a variant of HCM that is characterized by thickening of the left ventricular (LV) apical walls with loss of tapering from base to apex and obliteration of the LV apical cavity during systole, creating the typical spade-like configuration. Diagnostic criteria for apical HCM include an absolute apical wall thickness of > 15 mm or a ratio comparing apical LV and basal LV wall thicknesses of 1.3 to 1.5.
Although echocardiography is the first-line imaging modality for patients with suspected HCM, CMR has proved superior to echocardiography in detecting apical segment hypertrophy, she said.
Focus on case report
At the Milan meeting, Gezmis reported about the case of a lung cancer patient with focal cardiac FDG uptake on whole-body oncological PET/CT, which turned out to reflect apical HCM when further evaluated with CMR.
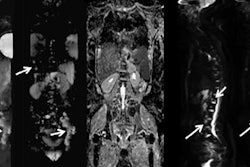
The 69-year-old woman was admitted to hospital with chest pain, dysarthria, and left-sided hemiparesis. Her head CT and head MR scans revealed no evidence of acute infarct, intracranial mass, or hemorrhage, but the chest x-ray showed an incidental mass in the lower zone of the right lung. A contrast-enhanced thoracic CT scan demonstrated a spiculated mass (31 x 29 x 24 mm in size) with a low attenuation center. There was also a 10-mm right hilar node, but no evidence of satellite lung lesions or pleural thickening. The appearances were thought to be consistent with primary lung malignancy, the radiological staging of which was T1b, N1, M0, she added.
A subsequent whole-body FDG-PET/CT scan showed uptake in the mass and right hilar lymph node, confirming the diagnosis, but increased focal activity was also noted at the apex of the left ventricle, which appeared to be within the wall rather than the lumen. This raised the possibility of cardiac metastasis, which would have changed the management of the patient, and further evaluation was required.
Despite the fact it was not ECG-gated, the thoracic CT scan was reassessed regarding the heart by putting the images into true cardiac planes using multiplanar reconstruction. This demonstrated the loss of tapering of myocardium from the base to the apex with thickening of distal walls, suggesting apical HCM.
Contrast-enhanced cardiac MRI was performed to rule out metastasis and validate the apical HCM diagnosis. The images showed disproportionate and focal wall thickening in the left ventricular apex, which corresponded with the area of avidity on the PET/CT scan. There was also a "spade-like" configuration of the apical left ventricular cavity, and contractility of myocardium was preserved.
 Dr. Stephen Harden.
Dr. Stephen Harden.
"No mass or gadolinium enhancement was noted and the appearance was in keeping with an apical hypertrophic cardiomyopathy phenotype. The pathology test results from the CT-guided biopsy of the lung mass and subsequently performed right lower lobectomy were adenocarcinoma. The benefit of chemotherapy was outweighed by risk and the patient has been under follow-up since then," Gezmis concluded.
Dr. Stephen Harden, a consultant cardiothoracic radiologist from University Hospital Southampton National Health Service (NHS) Trust, U.K., was a co-author of the research.
The group's full presentation from the ESCR 2017 meeting is available in the European Society of Radiology's EPOS database. To view it, click here.