Bone measurements on routine x-ray exams acquired before hip replacements can help identify patients at high risk for fractures related to the implants, according to a study published June 20 in the Journal of Arthroplasty.
Orthopedic surgeons in New York City studied cortical bone thicknesses on preoperative x-rays of total hip arthroplasty (THA) patients. They found the measurements were related to a higher risk for periprosthetic fractures, which could help clinicians manage these patients more effectively.
"Both major and [antero-posterior] cortical thickness indices are promising tools for identifying patients who are at high risk of [periprosthetic fractures] in the THA population," wrote a group led by senior author Dr. Joseph Lane, chief of metabolic bone disease services at the Hospital for Special Surgery.
An estimated 500,000 total hip arthroplasty procedures are performed each year in the U.S., with demand growing as a large segment of the population ages. In the next decade, joint replacements are expected to become among the most common elective procedures.
Direct fracture risk estimates are challenging for many hip replacement patients due to a lack of bone mineral density data, given that dual-energy x-ray absorptiometry (DEXA) scans are rarely done for THA patients, according to the authors.
In addition, DEXA scans using bone mineral density data are used to establish Fracture Risk Assessment Tool (FRAX) scores for patients, a gold standard for determining their future risk.
In this study, Lane and colleagues culled FRAX scores from 250 patients over the age of 50 who had hip replacements and 40 patients who had periprosthetic fractures. They then analyzed x-ray bone measurements -- namely, antero-posterior cortical thickness index (APCI) -- on preoperative x-rays from the patients. Finally, they analyzed correlations between the FRAX scores, the bone x-ray measurements, and periprosthetic fractures.
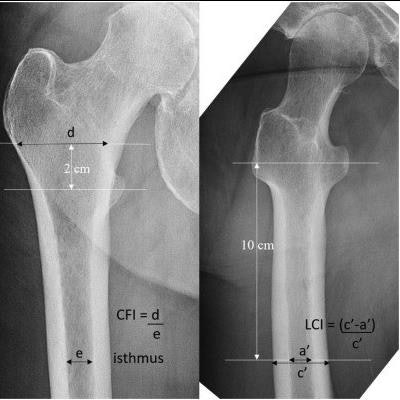
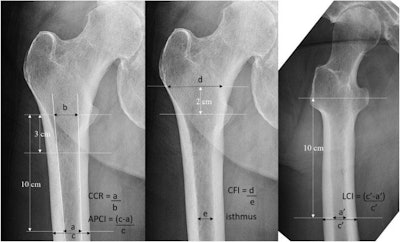 Measuring methods of each x-ray image of the hip: Canal to calcar ratio (CCR), AP cortical thickness index (APCI), canal flare index (CFI), and lateral cortical thickness index (LCI). Image courtesy of the Journal of Arthroplasty.
Measuring methods of each x-ray image of the hip: Canal to calcar ratio (CCR), AP cortical thickness index (APCI), canal flare index (CFI), and lateral cortical thickness index (LCI). Image courtesy of the Journal of Arthroplasty.According to the findings, higher FRAX scores were significantly associated with lower cortical thickness. Importantly, patients who had periprosthetic fractures after hip replacements had significantly higher FRAX scores (19.61 vs. 15.15 for FRAX major; 8.53 vs. 5.39 for FRAX hip) and significantly lower antero-posterior cortical thicknesses (0.52 vs. 0.55), the researchers stated.
"These findings indicate that cortical thickness measurements are a good proxy for fracture risk assessment in the THA population," they wrote.
That cortical thicknesses correlate well with FRAX scores and bone mineral density in both the hip and other locations isn't a new finding, with multiple studies demonstrating the connection, the authors noted.
However, no prior studies have focused on the people receiving total hip arthroplasty, who not only are at higher risk for fracture given poor bone health but also have the unique risk factor of undergoing THA, which can further decrease bone density, the researchers stated.
Thus, ultimately, the findings further support the use of cortical thickness as a measurement of fracture risk, they wrote.
"[Cortical thickness measurements] could prove to be a valuable pre- and post-op risk assessment tool for THA patients, especially given the ease of measurement and the availability of hip x-rays," Lane and colleagues concluded.