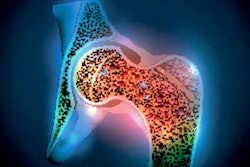
Bone mineral density (BMD) x-ray exams should be performed regularly in patients with psoriatic arthritis as they face a higher risk of falls and fractures, a team of Hungarian researchers has found.
Investigators at the University of Debrecen explored the differences between psoriatic arthritis patients and healthy controls concerning BMD, falls, and related fractures. They found lower BMD in psoriatic arthritis patients -- which predisposes them to a higher risk of injuries.
"Checking BMD regularly and starting primary prevention should be seriously considered in [psoriatic arthritis] patients," wrote first author Dr. Andrea Halasi, a rheumatology resident. The study was published January 17 in the Journal of Dermatology.
Psoriatic arthritis affects about 30% of people with psoriasis, a skin disease that causes a rash with itchy, scaly patches. While rheumatic disorders such as rheumatoid arthritis are known to increase bone loss and subsequently increase fracture risk, to date only controversial data have been published on the relationship between bone loss and psoriatic arthritis, according to the authors.
To elucidate the issue further, the researchers culled medical reports of 61 psoriatic arthritis patients and 69 age-matched control patients who underwent bone scans at their hospital between September 2021 and March 2022. The control group included randomly assigned age-matched patients referred by their attending physician for osteoporosis screening. Halasi's team tracked BMD data, 10-year fracture risk calculated with FRAX (a clinical fracture risk assessment tool), the number of low-impact prevalent fractures, and the frequency of falls.
The study found that femoral neck bone density, as well as vertebral and femoral neck T-scores, were lower and 10-year risk of hip fracture was higher in the psoriatic arthritis group. Psoriatic arthritis patients were more predisposed to prevalent fractures (odds ratio, 3.42; reference 1), including peripheral fractures (odds ratio [OR], 2.26), and vertebral fractures (OR, 13.33), as well as falls (OR, 3.93), compared with controls.
| Fractures and falls in psoriatic arthritis and control groups | ||
| Measure | Controls | Psoriatic arthritis patients |
| Number of falls | 7 (10%) | 34 (56%) |
| Number of prevalent peripheral fractures | 17 (24%) | 38 (62%) |
| Number of prevalent vertebral fractures | 4 (6%) | 16 (26%) |
| Peripheral fractures | 13 (19%) | 21 (34%) |
| Vertebral fractures | 1 (1%) | 10 (16%) |
"Based on our results, [psoriatic arthritis] essentially predisposes to reduced bone density, falls, and related fractures," the authors stated.
Moreover, an analysis within the psoriatic arthritis group showed that scalp psoriasis and late-onset psoriasis were significantly associated with a greater number of prevalent fractures, and the number of falls per year correlated with late-onset psoriasis, they added.
Since this was the first study to assess the relationship between the specific properties of psoriatic arthritis and bone fractures or falls, further research is warranted, the authors wrote. Ultimately, the study underlines the importance of the cooperation between dermatologists and rheumatologists, the researchers wrote.
"Patients with late-onset psoriasis are more likely to suffer falls and related fractures, especially if their disease is characterized by the involvement of the hairy scalp and body folds," they concluded.