Virtual colonoscopy's accuracy is hard to verify because it is usually compared against the imperfect gold standard of optical colonoscopy.
In recent years some researchers have sought to circumvent this shortcoming by using segmentally unblinded colonoscopy as the reference standard -- meaning that the endoscopist is given the VC results for each colon segment after first examining the segment without the benefit of VC results. As a result, the segmentally unblinded reference standard benefits from the findings of both exams, which can be assessed separately.
In a new study from Italy, the radiologists went further, using the results of both VC and colonoscopy -- in addition to a second conventional colonoscopy exam -- as their reference standard. The study, though understandably difficult to recruit for because it required back-to-back colonoscopies in addition to VC, might nevertheless have achieved the best reference standard so far for VC -- and is likely to pay off in terms of diagnostic quality for its intrepid subjects as well.
In the end, the accuracy of ultralow-dose VC on a four-slice scanner was comparable to that of conventional colonoscopy except in the smallest lesions, the team found. Conventional colonoscopy was significantly better for detecting such diminutive lesions, which are generally considered to be clinically insignificant.
"We have several studies that have demonstrated a miss rate for detection of polyps ranging from 15% to 31%," said Dr. Riccardo Iannaccone from the University of Rome "La Sapienza." "Therefore, in theory, false-positive findings at CTC (VC) could instead be false-negative findings at colonoscopy. And therefore the purpose of our study was to determine the diagnostic accuracy of low-dose MDCT using two sequential colonoscopies, so called back-to-back technique."
A pioneering study of back-to-back colonoscopies was published in 1997 by Dr. David Rex and colleagues from the Indiana University School of Medicine in Indianapolis. According to their results, colonoscopy's overall miss rate for adenomas was 24%, 27% for adenomas 5 mm or smaller, 13% for adenomas 6-9 mm, and 6% for adenomas 10 mm or smaller, the team reported (Gastroenterology, January 1997, Vol. 112:1, pp. 24-28).
On the other hand, the University of Rome study cohort underwent VC in addition to the two colonoscopies. (The first colonoscopy plus VC was performed the first day.) Eighty-eight patients completed the protocol, with 56.8% being symptomatic, Iannaccone said at the 2005 European Congress of Radiology in Vienna, Austria.
All subjects underwent a standard cathartic prep consisting of a polyethylene glycol solution and bisacodyl tablets, and an antiperistaltic drug (20 mg of Buscopan) was administered intravenously prior to CT. Manual room-air insufflation of the colon was performed to maximum patient tolerance.
CT images were acquired on a Somatom Plus 4 Volume Zoom scanner (Siemens Medical Solutions, Erlangen, Germany) with patients in the prone and supine positions. The previously optimized low-dose imaging protocol included 4 x 2.5-mm collimation, 3.0-mm slice thickness, 140 kVp, and an ultralow tube current setting of 10 mAs.
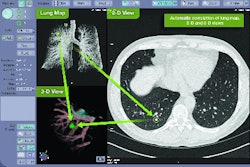
"Three independent radiologists analyzed the images on a dedicated workstation to assess the number, location, and size of all suspected polyps in a time-efficient manner, which means that when a suspected polyp was identified and magnified, 3D axial images, multiplanar reformations, and axial images were also added to the analysis," Iannaccone said. "We assessed sensitivity on both a per-polyp and per-patient basis. We also calculated sis for per patient analysis. We also calculated specificity, positive and negative predictive values, and interobserver variability."
Following CT, same-day conventional colonoscopy was performed by one of two staff endoscopists, who were blinded to the CT results. Polyps were not biopsied or excised at this colonoscopy, but saved for a second colonoscopy performed within two weeks of the first. For the second colonoscopy endoscopists had access to both of the previous exams, Iannaccone said.
According to the results of the second, unblinded exam, 42 patients had no polyps, while the remaining patients had 94 polyps, including 55 hyperplastic and 39 neoplastic lesions. Interobserver agreement was moderate to high on a per-polyp basis and high to excellent on a per-patient basis. The overall polyp miss rate for the first colonoscopy was 17%, in line with previous studies, Iannaccone said.
Overall per-polyp sensitivity was 62% for VC and 84% for colonoscopy. When only polyps 6 mm or larger were considered, VC and colonoscopy yielded per-polyp sensitivities of 85.6% and 83.8%, respectively. The per-patient analysis yielded a sensitivity of 80.4% for lesions of all sizes, compared to 93.5% for initial colonoscopy, and specificity of 74.6% versus 100% for initial colonoscopy. The positive predictive values for VC and initial colonoscopy were 77.6% and 100%, respectively. The negative predictive value was 77.7% for VC versus 93.3% for initial colonoscopy, the researchers reported.
The most frequent cause of false positives in VC was fecal material (12, 12, and 14 cases for readers 1, 2, and 3, respectively). These proved difficult to distinguish from polyps using the available equipment, Iannaccone said. (The institution has since implemented a 64-slice scanner.)
"Low-dose (VC) has a diagnostic accuracy similar to colonoscopy for the detection of polyps 6 mm in diameter or larger," he said. The relatively decreased performance of VC is correlated with relatively poor performance of the technique for the detection of small lesions. If we focus our attention on polyps on 6 mm or larger, we see that both techniques can reliably identify polyps."
By Eric Barnes
AuntMinnie.com staff writer
July 19, 2005
Related Reading
Prepless VC yields high sensitivity in average-risk subjects, June 10, 2005
Z-axis modulation cuts VC dose, keeps image quality high, April 12, 2005
Ultralow-dose virtual colonoscopy shows high sensitivity, April 8, 2003
Copyright © 2005 AuntMinnie.com