Recent virtual colonoscopy studies are stark proof of the power of acquisition protocols to affect sensitivity, according to a leading VC researcher. When the virtual exam is performed correctly, he said, its accuracy rivals that of conventional colonoscopy. When the protocol is wrong, the results are unacceptable.
At the 2005 International Symposium on Multidetector-Row CT in San Francisco, Dr. Patrick Rogalla from Berlin's Charité Hospital said the chasm separating excellent study results such as those of Pickhardt et al (91.5% sensitive for polyps 6 mm and larger) from the poor results typified by Cotton et al (40% sensitivity for polyps 6 mm and larger) is largely preventable. Pickhardt's group used 2.5-mm or 1.25-mm collimation in its multicenter trial (New England Journal of Medicine, December 2003, Vol. 349:23, pp. 2,191-2,200; Journal of the American Medical Association, April 14, 2004, Vol. 291:14, pp. 1,713-1,719).
While acknowledging several important differences between the two studies in terms of technique, including different training levels and 2D versus 3D interpretation, Rogalla asserted that the "primary difference was that the majority of patients were scanned using 5-mm slice thickness in the (Cotton) study, and it might have contributed to the difference in sensitivity."
Optimizing data acquisition protocols can ensure the best possible results in VC. "I will give you some tips so that your results will look like the Pickhardt study rather than the other ... studies," he said.
Thin-slice acquisition
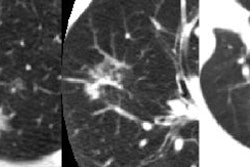
Collimation affects polyp visualization in important ways, Rogalla said, and it's clear that the smallest polyps benefit most from thin-slice imaging. "The question of whether you have to report them or not is a different story," he said.
For optimal sensitivity, radiologists should use the thinnest slices possible to cover the entire abdomen in a single breath-hold, Rogalla said.
Bowel prep
The best and driest bowel prep is the Phospho-soda formula (Fleet Pharmaceuticals, Lynchburg, VA), Rogalla said. Many VC researchers use a double dose to ensure thorough bowel cleansing. Still, he noted, the Food and Drug Administration has specifically issued an advisory noting a propensity for electrolyte disturbances when larger than normal doses are administered.
"Also, it has a terrible taste," he said.
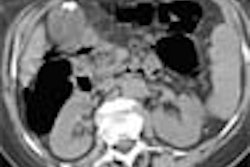
Prone and supine positioning
Scanning usually starts in the supine position, but prone scanning is also needed most of the time, Rogalla said. First, the efficacy of bowel distension should be assessed, if possible, from the scout acquisition. Most scanners have real-time reconstruction capabilities, and the bowel loops should be examined in a bone or lung window to ensure that they are fully distended.
If fluid can be seen in the colon, the patient must be turned to the prone position for a second acquisition to ensure that fluid-filled segments can be interpreted later, he said.
Premedication
The efficacy of administering glucagon or Buscopan (Boehringer Ingelheim, Ingelheim, Germany) before scanning to improve colonic distension is probably the most controversial aspect of virtual colonoscopy practice, Rogalla said. First a study by Yee et al showed that glucagon had no effect on bowel distension (American Journal of Roentgenology, July 1999, Vol. 173:1, pp. 169-172).
A study by Morrin et al two years later also found that glucagon did not improve distension (European Radiology, March 2002, Vol. 12:3, pp. 525-530). And a study by Bruzzi et al came to the same conclusion about Buscopan (European Radiology, August 27, 2003, Vol. 13:10 pp. 2,264-2,270), though other researchers have disagreed with these conclusions.
"The problem with those well-done studies is that they had a very low statistical power (< 25%)," Rogalla said. "So we opted to analyze our own data."
In a study of 240 patients who underwent virtual colonoscopy, Rogalla and colleagues found that glucagon improved distension significantly only when the results were analyzed per segment (p = 0.37 per segment versus p = 0.17 per patient). However, Buscopan was highly beneficial both on per-patient (p < 0.006) and per-segment analysis (p = 0.004). Buscopan also provided much better volume distension results than glucagon (4.23 versus 3.98), and significantly reduced the number of collapsed colonic segments (n = 11 for Buscopan versus n = 23 for glucagon). Still, he noted, Buscopan is not authorized for virtual colonoscopy in the U.S.
Automated insufflation
Distension is crucial in CT colonography (VC) applications; even large polyps cannot be seen in a collapsed colon segments, Rogalla said. The use of an automated insufflation device (PROTOCO2L, E-Z-EM, Lake Success, NY) can improve insufflation significantly by maintaining constant CO2 pressure during scanning.
"If you look at the data, you'll find that volume distension, and in particular the number of collapsed segments, (yield) significant improvement using automatic insufflation. So whenever you have the choice, I can recommend using the automated device."
Low-dose CT
Dose is an important issue for an exam such as virtual colonoscopy -- an exam that is administered to a large population with a low prevalence of disease, Rogalla said. Fortunately there are several studies showing that good virtual colonoscopy data can be acquired at very low doses. A study by van Gelder et al simulated ultralow-dose scanning down to the equivalent of 0.4 mAs, he said (Radiology, July 2002, Vol. 224:1, pp. 25-33).
"No scanner can actually perform it," Rogalla said of the van Gelder study. "But it shows the colon is a high-contrast object, so you can reduce the dose, and I would always recommend using low-dose protocols.... You can go down as low as 20 or 17 mAs in most patients."
IV contrast for problem-solving
The use of contrast is another source of controversy in virtual colonoscopy. A well-performed study of 200 patients by Dr. Martina Morrin and colleagues found that sensitivity improved from 58% to 75% with the use of IV contrast, Rogalla said. One clue to the group's results, he said, is that only 19% of the patients in the study had sufficient bowel prep (Radiology, July 2003, Vol. 228:1, pp. 152-156).
"What it tells us is that IV contrast is very helpful if you have poor preparation of the patient," he said. "IV contrast should be used as a problem-solving tool."
Fecal tagging
"Fecal tagging is a very promising tool not only to label the fluid, that is an easy task, but also to label the sticky stool that glues in particular in the ascending colon," Rogalla said. No bowel preparation technique can get rid of this type of stool, but tagging agents can mark it effectively. And once it is tagged, various digital cleansing techniques can be applied to digitally subtract the tagged stool from the surrounding mucosa.
"Viatronix (Stony Brook, NY) and other companies are now adapting this principal" to their interpretation tools, Rogalla said, projecting an image of a polyp that could be seen only after the tagged stool had been digitally removed.
"Fecal tagging is going to be a great help -- in particular with the new workstations," he said.
By Eric Barnes
AuntMinnie.com staff writer
August 24, 2005
Related Reading
CT colonography sensitivity low, April 14, 2004
Group credits 3D reading for best-ever VC results, October 15, 2003
Ultralow-dose VC appears feasible, August 3, 2004
Gastroenterology warning: Prepare for VC or regret it, October 6, 2004
VC faces off (again) against second-look colonoscopy, October 4, 2004
Copyright © 2005 AuntMinnie.com