CT-based coronary artery calcium (CAC) screening in individuals at intermediate risk of heart disease is probably cost-effective for men but not women, according to a new analysis in the October 11 edition of the Journal of the American College of Cardiology.
Based on a data analysis model that compared various strategies for reducing the risk of cardiac events over 10 years -- including preventive care such as CAC scoring with CT, universal statin therapy, or drug therapy only for individuals with high Framingham risk scores -- CAC scoring fell just under the traditional threshold of cost per quality-adjusted life-year (QALY) in men to make the technique cost-effective.
The picture is different for women, however.
"For women at intermediate risk for [coronary heart disease], CT screening does not seem to be cost-effective," wrote study authors Bob van Kempen, Sandra Spronk, PhD, and colleagues from Erasmus Medical Center and several other centers in Europe. That equation was maintained even at willingness-to-pay thresholds higher than the traditional $50,000 per QALY which showed that CT calcium screening was cost-effective in fewer than 20% of the model simulations (JACC, October 11, 2011, Vol. 58:16, pp. 1690-1701).
According to an accompanying editorial by Dr. Philip Greenland and Dr. Tamar Polonsky, "The evidence favoring routine CAC scoring from this trial, also based on the Rotterdam study data, is intriguing but not compelling enough yet to apply CAC screening to all individuals at moderate risk. A screening trial with CAC measurement is long overdue" (pp. 1702-1704).
Recent studies have shown that CT calcium scoring is a strong predictor of cardiovascular heart disease (CHD) that is independent of the Framingham risk score. In particular, the recent Rotterdam study, which examined more than 2,000 individuals at intermediate risk and showed that CAC scoring alone changed the CHD risk levels independent of Framingham risk score, has generated new interest in evaluating the predictive value and cost-effectiveness of CAC.
In their analysis, van Kempen and colleagues aimed to assess the cost-effectiveness of screening asymptomatic individuals at intermediate risk of coronary heart disease for coronary artery calcium with CT.
The group developed a Markov model based on the Rotterdam study results. Based on the model, they evaluated four strategies for reducing the risk of cardiac events:
- Current practice: The reference strategy, reflecting the incidence of CHD and non-CHD events of individuals at intermediate risk without preventive intervention, as observed in the Rotterdam study.
- Current guidelines: Based on full implementation of the most recent guidelines on the prevention of CHD; includes lifestyle advice for all, statin therapy when low-density lipoprotein (LDL) cholesterol is greater than 130 mg/dL (3.37 mmol/L), and antihypertensive medication when baseline systolic blood pressure exceeds 140 mm Hg.
- CT calcium screening: CT screening for coronary calcium in all individuals at intermediate risk.
- Statin therapy: Statin therapy for all individuals at intermediate risk.
Asymptomatic individuals at intermediate risk of coronary heart disease were simulated in the model over their remaining lifetime. QALYs, costs, and incremental cost-effectiveness ratios (ICERs) were calculated.
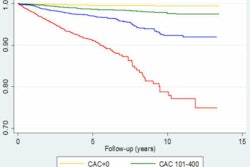
The results in men showed that CT screening for CAC was more effective, but more costly, than the other three strategies. The ICER of CT calcium screening was $48,800 per additional QALY, versus $30,278 per QALY for statin therapy.
Cost-effectiveness of CT CAC screening in men
|
Among women, however, implementing current guidelines had a lower cost per additional QALY, at $33,072, than CT screening at $35,869 per QALY, the group reported. CT screening was more effective and more costly than statin therapy, at $23,910 per additional QALY.
Cost-effectiveness of CT CAC screening in women
|
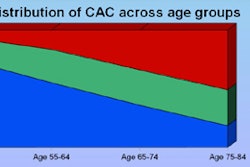
The two cohorts had some differences. Analysis of the baseline characteristics of the intermediate-risk cohort showed that the women were older than the men and had less-favorable risk factor levels, except for smoking and calcium scores, the authors noted.
Implementing current guidelines in men led to a steep increase in the number of statin users (from 12% to 75%) and antihypertensive users (from 23% to 64%), compared with current practice. The trend was similar in women, with statin users increasing from 15% to 87% and antihypertensive users increasing from 52% to 84%.
Factoring in generic drug prices made CT screening more cost-effective in men, with an incremental cost-effectiveness ratio of $24,675 per QALY, and generic drugs made implementation of current guidelines more cost-effective, with an ICER of $21,140 per QALY.
"Substituting the statin therapy strategy with the aggressive medical treatment strategy did not change the optimal decision in men," van Kempen and colleagues wrote. "In women, the optimal decision switched from current guidelines to aggressive medical treatment."
In men, the ICER for CT screening fell "just below the willingness-to-pay threshold of $50,000/QALY, and small changes in assumptions changed CT screening from being cost-effective to not cost-effective," van Kempen and colleagues wrote. Acceptability curves created from the data showed that "in a minor but substantial proportion of the simulations, CT screening was not cost-effective. However, with generic drug prices the ICER for CT screening dropped, and the result was more robust in sensitivity analysis."
In women, however, "CT screening was not found to be cost-effective, even after using a wide range of varying assumptions, which included assumptions more favorable to the CT calcium screening strategy by treating individuals in the higher end of 'low risk' (5% to 10% risk) more aggressively and with more treat-prone LDL thresholds," the group wrote.
The difference in the optimal decision between men and women can be explained by noting that compared with men, "more women were reclassified to the low-risk group, leading to less aggressive treatment," the authors wrote."Furthermore, within the low-risk group, the observed risk of CHD is higher in women than in men, so the foregone benefit with less aggressive treatment is higher in women. The benefit of CT screening is obtained in the high-risk group, where individuals are treated more aggressively compared with current guidelines for treatment of intermediate-risk individuals."
Because fewer women were reclassified to high risk by CT screening, its potential benefits were lower than in men, they wrote. Aspirin served to reduce the cost-effectiveness of CT screening even further in women because it is prescribed in men at high risk but not in women, due to doubts about its effectiveness in preventing coronary heart disease.
Among the limitations of the study, the recommendations apply only to individuals at intermediate risk of disease, the authors noted. They emphasized that the differences between the various strategies in terms of quality-adjusted life-years were small.
In their editorial, Greenland and Polonsky noted that given the shortcomings and conflicting outcomes of previous studies, more research is needed before any change in treatment strategy -- including to CT screening -- is implemented.
"With the residual uncertainty in this important area of preventive medicine, we believe that the only way to determine the 'best' strategy is to conduct a clinical trial with CAC testing to select patients for more or less intensive treatments," Greenland and Polonsky wrote. The study would be logistically challenging and would require a large number of patients who were followed for several years, they stated.
"However, in the absence of such a trial, the options seem to be so close to one another on careful analysis that reasonable errors in the assumptions can lead to very different conclusions," the editorialists wrote. "We conclude that there is not enough evidence, even with the newer data on risk reclassification, to justify a change in current clinical practice recommendations. A screening trial with CAC measurement is long overdue."