VIENNA - The new model-based iterative reconstruction (MBIR) technique handily outperformed adaptive statistical iterative reconstruction (ASIR) in one of the first head-to-head series, researchers reported on Saturday at the European Congress of Radiology (ECR).
In CT images acquired at nearly 80% dose reduction from standard protocols, MBIR significantly improved image quality compared to ASIR, though a couple of image quality measures, such as motion artifacts and increased blotchy appearance, actually worsened with the new technique, said Dr. Masaki Katsura from the University of Tokyo.
MBIR is more advanced than ASIR, as it is a pure iterative reconstruction technique that does not involve blending with filtered back-projection (FBP) images. It also incorporates both statistical and optical analysis, Katsura said. Not only is there little data available resulting from MBIR in clinical use, there are no direct comparisons of MBIR with ASIR (both from GE Healthcare), he said.
"The purpose of our study was to compare the image quality of MBIR and ASIR in the same patients," Katsura said in his presentation.
Their prospective study looked at 100 patients (55% men; mean age, 65.6 ± 12.4) scheduled for standard unenhanced chest CT. Each patient underwent both a standard-dose and a low-dose exam on a 64-detector-row scanner (CT750HD, GE Healthcare), with both exams utilizing tube current modulation and fixed noise indices (11.1 at 5 mm for standard-dose CT; 24.82 for low-dose CT). The rest of the CT parameters were held constant for the two exams, including 120 kVp and 64 x 0.625 mm. The investigators used an ASIR/FBP blend of 50% to compare with the MBIR images. Standard-dose CT had a noise index of 31.5 at 0.625 mm, compared with a noise index of 70.44 for low-dose CT, Katsura said.
For subjective image analysis, the radiologists examined 300 randomized image datasets with the two radiologists blinded to the results. They evaluated the overall graininess of the parenchyma on a five-point scale (five being the worst); artifacts including motion artifacts, streak artifacts, and a pixilated blotchy appearance on a three-point scale (three signifying substantial artifacts); and overall diagnostic acceptability on a four-point scale. They also measured objective image noise in the lung parenchyma. Data were analyzed using the sign test and paired Student's t-test.
The results showed a 79% decrease in the low-dose (0.85 mSv) compared to the reference dose (4.04 mSv) acquisition, Katsura said. "Our low-dose values were comparable with low-dose CT in the National Lung Screening Trial." For patients weighing 65 kg to 75 kg, the reference dose was 5.4 mSv, compared with 1.13 mSv for the low-dose scans, he said.
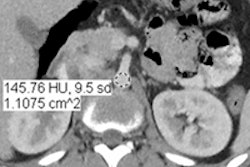
As for readability, low-dose MBIR images had significantly lower objective image noise in the lung parenchyma (16.93 ± 3.00), compared with low-dose ASIR (49.24 ± 9.11, p < 0.01) and standard-dose ASIR images (24.93 ± 4.65, p < 0.01).
Streak artifacts were minimal with MBIR, demonstrating mixed results between the readers. However, "motion artifacts were more prominently seen with low-dose MBIR images, in some cases at least," he said. "Pixilated blotchy appearance was also a problem seen with low-dose MBIR in almost every patient."
Overall diagnostic appearance was "fully" or "probably" acceptable for every case in low-dose MBIR, versus "fully" acceptable in ASIR for reader 1, again showing mixed results, Katsura said.
"So image noise and streak artifacts significantly improved with MBIR, and low-dose MBIR images were all diagnostically acceptable," he said. But "motion artifacts were more prominent in MBIR, which may reflect the differences in time resolution [between the techniques], which has to be investigated."
"Pixilated blotchy appearance was also more prominent with MBIR," a phenomenon that also needs more investigation, but which may improve with subsequent versions of the software, he said.
"Actually, pixilated blotchy appearance has been described in many initial ASIR reports, but it's not a problem seen in our ASIR images, which, according to the vendor, is due to recent advancements of the ASIR algorithm itself -- so we hope the same thing happens for MBIR." In any case, the readers found them "not overly distracting" and they didn't affect the diagnosis, Katsura said.
Finally, low-dose MBIR produced a steplike appearance at tissue interfaces (pulmonary fissures, small pulmonary vessels, bronchi, etc.), which, again, were not too distracting and didn't affect diagnostic acceptability of the images, according to Katsura.
Overall, MBIR showed greater potential than ASIR in low-dose CT, Katsura concluded, with dose almost equivalent to the low-dose standard in the U.S. National Lung Screening Trial. That kind of dose reduction makes it promising for imaging infants or young children, as well as for lung cancer screening purposes, he said.
Right now the biggest issue impeding routine clinical use is MBIR's one-hour processing time for each patient -- too long for acute care or other time-sensitive applications, Katsura said.