VIENNA - The German Competence Network of Congenital Heart Defects estimates that 1 in every 100 babies is born with a heart defect. The number of babies with congenital heart disease (CHD) each year remains constant across Europe, and about 6,000 babies are expected to have CHD each year, but thanks to progress in medicine, most of these babies now survive to adulthood.
In these patients, imaging can assist the cardiac surgeon in many ways, and it's critically important for radiologists to become familiar with the most common surgical procedures of CHD, as well as the imaging aspects, believes Dr. Michael Hübler, chief physician in the department of pediatric cardiac surgery at Kinderspital in Zürich.
 The use of MRI to document the effects of congenital cardiac diseases is poised for growth, according to Dr. Michael Hübler from Zürich.
The use of MRI to document the effects of congenital cardiac diseases is poised for growth, according to Dr. Michael Hübler from Zürich.
"We expect a considerable increase of such patients due to the fact that more than 90% now reach adulthood and also because conventional x-ray, ultrasound, CT scanning, and MRI remain principal investigational tools to diagnose congenital heart defects, as well as to diagnose consequent changes following a surgical or interventional repair," said Hübler, who will elaborate on this topic during this afternoon's special focus session.
Examples of ways in which imaging can assist these patients are by quantifying atrial and ventricular volumes consequent to pulmonary regurgitation, defining the extent and site of stenosis of the aorta or the pulmonary arteries, and determining the extent of pulmonary vein stenosis or anomalous insertion of the pulmonary vein. It can also help to define the anatomy of the coronary arteries in patients who have undergone an arterial switch operation, Ross procedure or tetralogy of Fallot correction. Yet until fairly recently, there has been little structured, advanced training for nonspecialist doctors who look after grown-up congenital heart (GUCH) patients. The number of patients remains relatively low, so this type of training has only been possible at a few institutions, he explained.
Because some GUCH patients have postoperative difficulties that require imaging, Hübler thinks it is important for radiologists to be able to identify and assess complications of typical problems, such as dilatation of the right ventricle due to severe pulmonary regurgitation, residual or recurrence of stenosis in the aortic arch and isthmus (coarctation), and dilatation of the previously operated aortic root (post Ross procedure). A cardiac emergency may occur in an imaging suite, and radiologists and radiographers need to be aware of such events.
"If a patient with an uncorrected cardiac defect, a palliated congenital heart defect, or severely decreased cardiac function attends for an MRI examination, the patient may become decompensated after only administration of anesthesia or injection of radiopaque fluid," he noted. "A cyanotic patient with significant residual defects may also decompensate both hemodynamically and in terms of oxygen saturation and CO2 washout as a result of anesthesia."
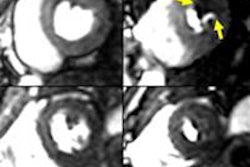
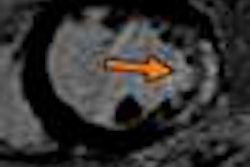
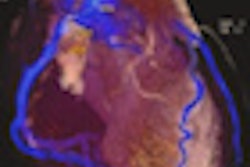
 A 57-year-old man with vascular ring, "double aortic arch," huge Kommerell's diverticulum, and aneurysm of the descending aorta. Dysphagia and increasing diameter of the diverticulum can be seen. Images courtesy of Dr. Michael Hübler.
A 57-year-old man with vascular ring, "double aortic arch," huge Kommerell's diverticulum, and aneurysm of the descending aorta. Dysphagia and increasing diameter of the diverticulum can be seen. Images courtesy of Dr. Michael Hübler.Despite these concerns, the future of imaging in GUCH looks set to rapidly evolve, and the use of MRI for diagnostic purposes is likely to increase. Also, MRI may be used as a screening tool to examine the status of relocated coronaries (e.g., after arterial switch or the Ross procedure), and it may replace some invasive catheter-based diagnostic investigations. The use of MRI to document the effects of congenital cardiac diseases and the therapeutic maneuvers on development of the brain is poised for growth, according to Hübler. It will be interesting to see if MR-based interventional procedures can be developed further, particularly to see if flow phenomenon and computerized models can be developed to achieve the best hemodynamic results, he added.
 Patients with congenital heart disease can benefit from evaluation with newer MR sequences and postprocessing tools such as 4D flow assessment, believes Dr. Matthias Gutberlet from Leipzig, Germany.
Patients with congenital heart disease can benefit from evaluation with newer MR sequences and postprocessing tools such as 4D flow assessment, believes Dr. Matthias Gutberlet from Leipzig, Germany.
"Due to the very often quite complex anatomy, imaging is a crucial part of these follow-up examinations. Invasive procedures and radiation exposure in young patients should be avoided whenever possible," commented Dr. Matthias Gutberlet, a professor of cardiac imaging at the University of Leipzig in Germany. "Usually in children, noninvasive imaging is done by Doppler echocardiography, but when children become older and reach adulthood, the access to visualize especially the right ventricle and right ventricular outflow tract becomes increasingly difficult due to a limited acoustic window or changed anatomy. Therefore, cross-sectional imaging, mainly cardiac MRI (CMR) but more and more also cardiac multidetector CT, comes into the game."
Most GUCH defects can be corrected by interventional or surgical procedures, which are usually performed as early as possible during childhood or infancy. The goal of these procedures is to reconstruct normal physiology and anatomy, if possible. Very often, the reconstruction of normal anatomy and physiology cannot be achieved or only palliative surgical procedures can be performed and therefore the effects (i.e., volume and/or pressure overload, etc.) of that pathologic physiology and anatomy require lifelong follow-up examinations.
"Besides depicting the underlying pathology in CHD, CMR is capable of assessing more than simple anatomy; it can assess ventricular function, muscle mass, scar detection, and even flow velocity and shunt quantification. This is especially important for patients with congenital heart disease, who can benefit from the evaluation with newer MR sequences and postprocessing tools like 4D flow assessment," he noted. "It is anticipated that the number of patients for whom these methods are beneficial is continuously increasing due to the progress in treatment and diagnosis."
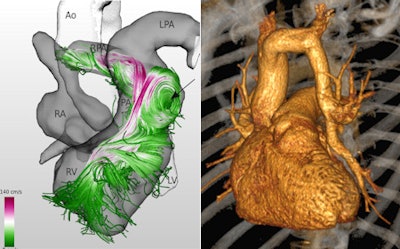 Left: MR 4D flow reconstruction of an adult patient after surgically corrected tetralogy of Fallot demonstrates an aneurysm of the right ventricular outflow tract with pathologic flow pattern (arrow) due to the aneurysm and pulmonary valve regurgitation. RV=right ventricle, LV=left ventricle, RA=right atrium, LPA=left pulmonary artery, RPA=right pulmonary artery, Ao=aorta, PA=pulmonary artery. Adapted from: Born S, Pfeifle M, Markl M, Gutberlet M, Scheuermann G. Visual Analysis of Cardiac 4D MRI Blood Flow Using Line Predicates. IEEE Trans Vis Comput Graph 2012. Right: 3D reconstruction of a multidetector-row CT dataset of a 65-year-old patient with a partially anomalous left pulmonary vein. Images courtesy of Matthias Gutberlet.
Left: MR 4D flow reconstruction of an adult patient after surgically corrected tetralogy of Fallot demonstrates an aneurysm of the right ventricular outflow tract with pathologic flow pattern (arrow) due to the aneurysm and pulmonary valve regurgitation. RV=right ventricle, LV=left ventricle, RA=right atrium, LPA=left pulmonary artery, RPA=right pulmonary artery, Ao=aorta, PA=pulmonary artery. Adapted from: Born S, Pfeifle M, Markl M, Gutberlet M, Scheuermann G. Visual Analysis of Cardiac 4D MRI Blood Flow Using Line Predicates. IEEE Trans Vis Comput Graph 2012. Right: 3D reconstruction of a multidetector-row CT dataset of a 65-year-old patient with a partially anomalous left pulmonary vein. Images courtesy of Matthias Gutberlet.Originally published in ECR Today on 9 March 2013.
Copyright © 2013 European Society of Radiology