The economics of CT lung cancer screening measure up to other population-based screening programs such as mammography in terms of cost-effectiveness, according to an analysis of data from the National Lung Screening Trial (NLST) that was presented on Monday at a U.S. National Cancer Institute (NCI) meeting.
This follow-up analysis of NLST data found that a low-dose CT lung cancer screening program based on NLST criteria and methods would meet generally accepted criteria for the cost-effectiveness of a screening test. CT lung screening has a cost-benefit profile that compares favorably to mammography, and attendees at the meeting of NCI's board of scientific advisors and national cancer advisory board were generally positive about CT lung screening's impact.
"As a national cancer effort, we have been looking for a long time to find an effective screening procedure for lung cancer," said one attendee. "We have one now in front of us, and it's quite striking. So I think we should embrace and celebrate that."
Confirming NLST data
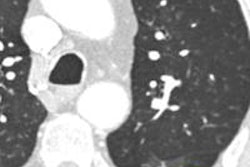
Data from NLST changed the debate over low-dose CT lung cancer screening when the information was released in 2011. The study found that screening reduced mortality by 20% in a population of current and former heavy smokers when compared to screening with chest x-ray, prompting widespread debate over if, when, and how CT lung screening could be rolled out to a wider population.
At Monday's meeting, the data on cost-effectiveness were presented by Dr. Bill Black, a thoracic radiologist at Dartmouth University who was an investigator with the American College of Radiology Imaging Network (ACRIN), which conducted one of the two arms of NLST.
Black's group examined data from the ACRIN arm and extrapolated it to the other arm of the trial, the Lung Screening Study. The group developed data on quality-adjusted life years (QALYs) for three different strategies: lung cancer screening with CT, screening with chest x-ray, and no screening at all. For purposes of the analysis, the researches assumed that chest x-ray was ineffective.
They found that while low-dose CT screening was the most expensive strategy of the three -- costing $1,600 more per person than no screening -- it produced the highest number of QALYs, or the number of years of life added due to an intervention. They then calculated the incremental cost-effectiveness ratio (ICER), or the cost in 2009 dollars that each QALY added to a screening subject's life.
| Cost-effectiveness of CT lung screening | |||
| Type of screening | Cost | QALYs | ICER in $ per QALY |
| Low-dose CT | $2,770 | 11.0143 | $72,916 |
| Chest x-ray | $1,730 | 10.9924 | NA |
| None | $1,170 | 10.9924 | NA |
The 0.0219 difference in QALYs between CT screening and chest x-ray/no screening looks small -- about a week of extra life across the entire study population. However, Black reminded meeting attendees that it represents the application of CT screening's benefit from the 4% of participants who had cancer to the entire population of NLST participants.
Black also pointed out that the CT costs include three rounds of screening, as well as the workup of true and false positives and the management of lung cancer. It does not include the cost of treating incidental findings.
"It's not my role to say what's acceptable, but I can just point out to you that it's pretty well-regarded in the medical literature by policymakers that this is in the acceptable range; less than $100,000 per QALY is considered acceptable," Black said. "There are a lot of things that we do that cost far more than that per QALY."
Black also pointed out the drawbacks of assuming that x-ray screening has no value. Data from the Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial actually found a slight mortality benefit to x-ray screening, but the difference was not statistically significant. If it is indeed the case that x-ray screening has a benefit, then CT lung screening's ICER would be even more favorable -- at around $50,000 -- compared to no screening.
Another major source of uncertainty is the "catch-up" phenomenon -- the fact that the number of lung cancer cases on chest x-ray would eventually catch up to the number found earlier on CT. The researchers assumed that all catch-up cases in the chest x-ray arm had appeared by the end of the study period. It's plausible that there could be another 20 to 40 catch-up cases appearing in the chest x-ray arm in the next few years, in which case CT's ICER estimate would fall to about $60,000.
"The two major sources of uncertainty in our analysis of the NLST data suggest that to the extent that our assumptions are incorrect, we have underestimated the cost-effectiveness within NLST," Black said.
Several remaining issues include whether the $300 cost of CT lung screening exams in NLST can be replicated in the real world, as well as the number of follow-up exams required for positive studies. NLST was very conservative, only performing one follow-up CT scan for every positive screening. Many other studies have performed four or five scans, Black said, which would boost the ICER over the key $100,000 threshold.
Who should be screened?
Finally, the biggest issue is who should be screened. For example, the entire population of all smokers older than age 18 has one-tenth the cancer risk of the older, heavier smokers in NLST, who had 30 pack-year smoking histories. Screening everyone with a smoking history would produce a cost-effectiveness ratio that is "prohibitively high," Black said. Screening efforts therefore should use the NLST criteria, he believes.
In discussing the new data, several in attendance at the meeting sought comparisons between the NLST results and the cost-effectiveness of other screening campaigns, such as for breast, prostate, and cervical cancer. With respect to mammography, CT lung cancer screening with the NSLT criteria compares favorably to mammography using the 50-year-old threshold at which breast screening begins, Black said.
"There were some eyebrows raised when they saw those [cost-effectiveness] figures," said Dr. Barry Kramer, director of the NCI's division of cancer prevention. "For approximately every 1,000 smokers and former smokers screened after about seven years, there will be three fewer deaths from lung cancer. Mammography -- remember you are screening average-risk women -- is worse than that, closer to one per 1,000 over 10 years or so."
The U.S. is already involved in screening efforts for average-risk populations that have a lower return on investment than CT lung cancer screening, Kramer continued. He cautioned, however, that the positive news about CT lung screening shouldn't blind smokers to the fact that the best way they can reduce their mortality risk is to stop smoking.
Gender and histology
The data on CT lung screening's cost-effectiveness were preceded by another secondary analysis of NLST data, one that looked at whether the effectiveness of screening varied according to factors such as gender or the histological makeup of the cancers that were found in the study.
Paul Pinsky, PhD, acting director of the NCI's early detection research branch, presented data that showed that CT lung screening appeared to have a slightly more beneficial effect on women than men. Women who were screened with CT had a relative risk of 0.73 of dying from cancer compared to those who received x-ray screening. That compares to a relative risk of 0.92 for men.
NLST data also showed that CT screening had a larger effect in reducing deaths among those with adenocarcinoma, with a relative risk mortality reduction of 0.75, compared with other cancers such as squamous cell (relative risk reduction of 1.23).
One meeting attendee pointed out that CT's effectiveness in women could be related to biology, while adenocarcinoma is known to respond well to chemotherapy. CT lung screening may simply be more effective in patients who have cancers for which there are effective therapies.
"Perhaps you can refine the data and be able to target who really benefits from this," the attendee said. "Because I think this is better than mammography, at least for women, and lung cancer is the No. 1 killer of women now."