Computer-aided detection (CAD) finds most cancers that were missed in CT lung cancer screening, according to a new study in Radiology. CAD can enhance the value of CT screening by finding these cancers in time to remove them surgically.
The study from Icahn School of Medicine at Mount Sinai and Peking Union Medical College in China was based on an analysis of 50 lung cancers, consisting of solid nodules that were initially missed in the International Early Lung Cancer Action Program (I-ELCAP) trial and then detected on a subsequent screening.
When the investigators applied four types of lung CAD systems to the earlier screenings, they detected 56% to 70% of the lesions that were originally missed. Still, CAD missed about one-fifth of cancers in the screening round when they were first identified by the radiologist (Radiology, March 28, 2016).
"We were able to demonstrate that CAD systems were able to identify a large proportion of cancers that were missed by radiologists in the context of lung cancer screening," wrote co-author Dr. David Yankelevitz in an email.
This is a necessary step in proving the usefulness of CAD in screening, he added.
Missed in initial screen
Dr. Mingzhu Liang, Dr. Wei Tang, and colleagues from Peking Union Medical College and Dr. David Yankelevitz, Dr. Claudia Henschke, PhD, and others from Mt. Sinai identified 50 lung cancers from the I-ELCAP study, found in patients recruited between 1994 and 2013. The tumors were missed on an initial lung screening exam (time 0), but they were visualized on subsequent screening exams (time 1).
Radiologists going back to time 0 were able to see them at that time as well. All cases had pathologic confirmation and 44 underwent surgical resection, the authors wrote.
The reviews by two experienced radiologists were performed independently at both time points, and they noted the location and diameter for each cancer at each time point. Disagreements in interpretation were resolved by consensus.
Four CAD systems from four sources were used:
- CAD 1 -- Lung VCAR version 11.3-10.11 (GE Healthcare)
- CAD 2 -- ImageChecker CT version 8.3.12 (Hologic)
- CAD 3 -- syngo.via VA20 (Siemens Healthcare)
- CAD 4 -- Cornell Via (Cornell University)
Two radiologists independently interpreted the processed CAD images and determined whether to accept or reject each nodule candidate. Disagreements were resolved in consensus or by a third radiologist. The number of detected cancers was documented for each CAD for scans performed at time 0 and time 1.
Most cancers found
In every case, CAD detected most of the missed nodules. Among the 50 cancers missed by the radiologist at time 0, the four CAD systems detected 56% to 70%. At time 1, the detection rates ranged from 74% to 82%.
All cancers were smaller at time 0 (average, 4.8 mm) and had grown by time 1 (average, 11.4 mm), "which suggested that size was a determining factor in the performance of the human reader," the group wrote.
| CAD detection of nodules by system | ||||
| CAD system | ||||
| 1 | 2 | 3 | 4 | |
| CAD detection rate at time 0 | 56% | 70% | 68% | 60% |
| CAD detection rate at time 1 | 74% | 82% | 82% | 78% |
| Detections accepted by reviewing radiologists | 34.8% | 55.2% | 85.4% | 34.5% |
| No. of rejected detections per scan | 7.4 | 1.7 | 0.6 | 4.5 |
| No. of cancers detected after cancer was missed at time 0 | 28 | 35 | 34 | 30 |
Among the 50 missed cancers, CAD systems 1, 2, 3, and 4 detected three, six, four, and six cancers at time 0, respectively, but the systems did not detect that same cancer when it had grown at time 1.
"The performance of each of the CAD systems was different although not significantly," Yankelevitz wrote. "There were trade-offs in terms of some being more sensitive but having more false positives. Ultimately, we anticipate that all of the various systems will continue to improve and their usefulness in clinical practice will improve."
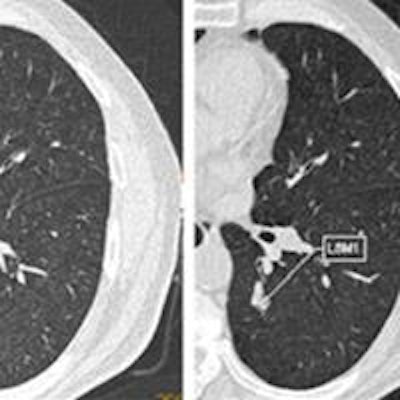
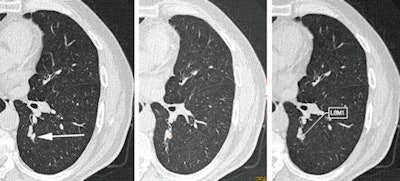 CT images of small cell carcinoma in the left lower lobe. At time point 0, when the lung cancer was small, it was missed by the interpreting radiologist (left, arrow), but it was detected by two of the four CAD systems (middle and right). Image republished with permission from RSNA, from Liang et al, Radiology, March 28, 2016.
CT images of small cell carcinoma in the left lower lobe. At time point 0, when the lung cancer was small, it was missed by the interpreting radiologist (left, arrow), but it was detected by two of the four CAD systems (middle and right). Image republished with permission from RSNA, from Liang et al, Radiology, March 28, 2016.Nodule size important
The CAD systems detected 0% to 17% of cancers smaller than 3 mm in diameter, 69% to 78% of those 3 mm to 6 mm in diameter, and 42% to 83% of those 6 mm or larger.
"Surprisingly, we found that three of the four CAD systems had better detection rates for the cancers that were 3 to 6 mm in diameter than for those that were 6 mm or more in diameter," the authors wrote. The likely reason is that CAD systems are designed to detect the small nodules that radiologists often miss.
Although high CAD sensitivity for cancer detection is necessary, it must be balanced against the false-positive rate to avoid unnecessary time and effort in eliminating false positives, they wrote.
Per the study design, CAD performance at time 0 was superior to that of radiologists, but at time 1, when all cases were identified by interpreting radiologists, CAD performance lagged, missing up to 26% of the cancers. Similar findings were reported in previous studies.
As for limitations, this largest-ever series had only 50 cases, which were taken from a variety of I-ELCAP sites and chosen solely because they were missed.
The findings also indicate that for now, CAD's best role remains as a second reader.
"We did not feel the sensitivity of CAD was high enough at the present time to be used before the radiologist reviews the exam and should remain primarily as a second read," Yankelevitz said.
Ultimately, CAD selection will depend on the radiologist's preference, he added. Some will opt for higher sensitivity and more false positives, while others will prefer a lower detection rate but fewer false positives.
As CAD systems advance, it will be important to establish quality standards for their performance, he noted.
"Part of this will include collecting a database of cases that are of particular necessity to add to the value of CAD, and the continued collection of cancers that were initially missed by radiologists will be a critical component for this type of database," Yankelevitz said.