Researchers from Colorado have proposed expanding the diagnostic criteria for chronic obstructive pulmonary disorder (COPD) to consider CT data along with a patient's symptoms, environmental exposure, and spirometry results in a study recently published in Chronic Obstructive Pulmonary Diseases: Journal of the COPD Foundation.
The current standard for diagnosing COPD, the Global Initiative for Chronic Obstructive Lung Disease (GOLD), largely depends on information drawn from pulmonary function tests, namely spirometry. Recent studies, however, have reported that COPD progression can vary widely and that many individuals who turn out to have COPD do not demonstrate structural changes detectable on early spirometry tests.
"If we diagnose COPD based only on impaired lung function, then we miss many patients in the early stages of the disease," senior author Dr. James Crapo of National Jewish Health in Denver noted in a statement released by the hospital. "While some physicians do empirically treat patients with symptoms, many patients are not getting therapy that can improve their symptoms, their quality of life, and might extend their lives."
To develop a more holistic approach to COPD diagnosis, Crapo and colleagues evaluated the cases of 8,784 current and former smokers who participated in the ongoing, large-scale Genetic Epidemiology of COPD (COPDGene) trial (Chronic Obstr Pulm Dis, November 2019, Vol. 6:5, pp. 384-399).
They identified four key disease characteristics that were associated with COPD in this cohort:
- History of cigarette smoking
- Clinical symptoms of dyspnea and/or chronic bronchitis
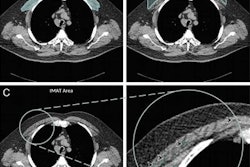
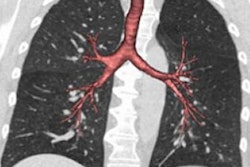
- Abnormal chest CT showing emphysema, gas trapping, and/or airway wall thickening
- Abnormal spirometry results (forced expiratory volume less than 80% and/or a ratio of forced expiratory volume to forced vital capacity of less than 0.7)
The researchers found that integrating these four criteria into COPD diagnosis would have flagged 82% of the participants as having an increased risk of reduced lung function and mortality, compared with only 46% of the patients using the GOLD criteria.
Further analysis revealed that trial participants who smoked and met two additional criteria had a 26% increased risk of losing significant lung function and a 28% increased likelihood of dying within five years compared with smokers who did not meet any additional criteria. Those who met all four diagnostic criteria had a 188% increase in risk of losing lung function and a roughly 500% chance of dying within five years compared with those who did not meet any additional criteria.
"Right now people who do not meet the current diagnostic criteria for COPD are not included in clinical trials of experimental COPD therapies," Crapo said. "Our proposed diagnostic criteria could open clinical trials to these people, stimulate important research of potential therapies to slow, stop or even prevent progression of the disease."
In an accompanying editorial, Dr. Peter Barnes of Imperial College London in the U.K. and colleagues noted that the studies confirmed that many smokers who do not have abnormal spirometry results, and thus do not meet the current criteria for further testing, are likely to develop serious COPD and have an increased risk of death.
"This new approach to diagnosis is easy to apply in hospital clinics, where CT scanning is readily available and many patients already have routine low-dose CT scans performed," Barnes and colleagues wrote. "However, it may be more difficult to implement in general practice, where most patients with early COPD are seen."