An artificial intelligence (AI) algorithm can provide fully automated quantification of emphysema, offering potential as a tool for image-based diagnosis and quantification of emphysema severity, according to research published online March 4 in the American Journal of Roentgenology.
After testing prototype AI software on over 140 patients, a multinational team of researchers found that the algorithm showed very strong correlation with traditional pulmonary function tests.
"The ability of an AI-based system to analyze high-dimensional image data and generate valuable clinical information without input from human observers should thus hold considerable potential for granular quantitative imaging approaches to provide patients with accurate diagnoses and steer treatment," wrote the team, led Dr. Andreas Fischer of the Medical University of South Carolina (MUSC) and the University Medical Center Mannheim in Germany.
Although several visual, semiquantitative, and quantitative techniques are used to assess emphysema, these methods are subject to increased interobserver and interpatient variability, according to the authors.
To see if AI could accurately quantify emphysema, the researchers used a deep image-to-image network -- a multilayer convolutional neural network that had been trained and tested on more than 10,000 CT datasets acquired on scanners from three vendors at over 20 clinical sites in the U.S. and Europe. Approximately 25% of these datasets were from patients with emphysema.
The algorithm was retrospectively evaluated on 141 patients who had received unenhanced chest CT and spirometry measurements within six months of each other at MUSC between August 2017 and July 2018. All CT exams had been acquired on one of three scanners from Siemens Healthineers: Somatom Definition Flash, Force, or Emotion.
To determine if reconstruction methods would impact performance, the researchers applied the algorithm to two reconstruction kernels. The first method used a section thickness of 1.5 mm with a long kernel, while the second utilized a section thickness of 1.5 mm with a soft-tissue kernel. Emphysema was quantified using spatial filtering and a threshold of -950 Hounsfield units.
The patients had a mean spirometry-based Tiffeneau index (TI) of 0.57. The first reconstruction method showed a mean percentage of emphysema of 9.96 ± 11.87%, while the second method had a mean percentage of 8.04 ± 10.32%.
The algorithm correlated very strongly with the TI on both the first (Spearman correlation coefficient = -0.86) and the second (Spearman correlation coefficient = -0.85) CT reconstruction methods. Both results were statistically significant (p < 0.0001).
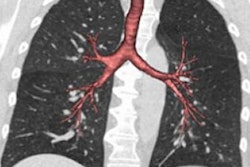
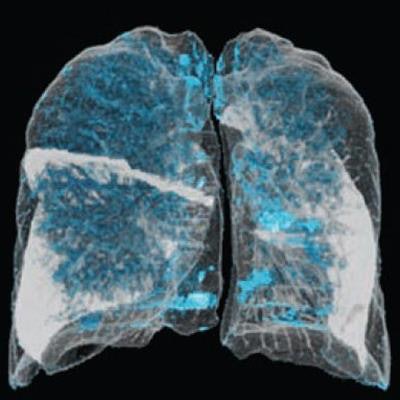
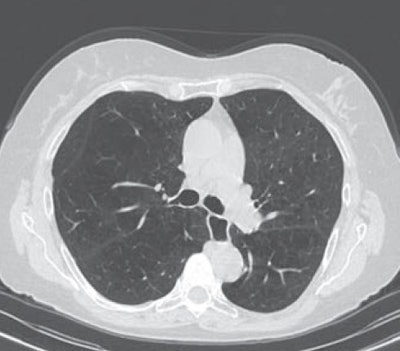 A 65-year-old man with severe lung emphysema (light blue on images below) seen on axial CT image (image 1 above), CT image including AI-based calculation (image 2), and 3D model (image 3). Extent of low-attenuation volume is seen inside green outline in both lungs in image 2. Purple outline in anterior right part of image 2 marks boundary between upper and middle lobes. Gray outline in image 2 correctly segments lower part of upper lobe and ensures that all lung tissue was considered. Also in image 2, orange outline denotes margin of tracheobronchial tree, and blue outline denotes margin of left lower lobe. All images courtesy of the AJR.
A 65-year-old man with severe lung emphysema (light blue on images below) seen on axial CT image (image 1 above), CT image including AI-based calculation (image 2), and 3D model (image 3). Extent of low-attenuation volume is seen inside green outline in both lungs in image 2. Purple outline in anterior right part of image 2 marks boundary between upper and middle lobes. Gray outline in image 2 correctly segments lower part of upper lobe and ensures that all lung tissue was considered. Also in image 2, orange outline denotes margin of tracheobronchial tree, and blue outline denotes margin of left lower lobe. All images courtesy of the AJR.Those results indicate that AI-based emphysema quantification meaningfully reflects clinical pulmonary physiology, according to the researchers.
"Further investigation is needed to establish quantified AI-based emphysema analysis as a potential biomarker for patients with COPD, thus improving diagnostic performance for a specific outcome and maximizing information retrieval to better understand the causes of disease," the authors wrote. "Thus, AI-based pulmonary emphysema diagnostics could contribute to complementary phenotyping as part of an imaging biomarker for patients with COPD to shape the individual therapy of patients as a common diagnostic tool, in combination with pulmonary function tests."