CT pulmonary angiography (CTPA) findings suggest that the development of pulmonary thromboembolism (PTE) in patients with COVID-19 is a manifestation of pulmonary artery thrombosis due to lung inflammation rather than venous thromboembolism, according to a study published July 9 in Radiology: Cardiothoracic Imaging.
The findings offer a working hypothesis in a clinical question regarding COVID-19 that has remained unclear, wrote a team led by Dr. Enrico Cavagna of Ospedale Infermi in Rimini, Italy.
"[Our] findings are in keeping with other observations showing that COVID-19 triggers a hypercoagulable state, and also contribute to the discussion between pulmonary artery thrombosis versus venous thromboembolism as potential hypotheses for this phenomenon," the researchers wrote.
Blood coagulation is a common finding among hospitalized patients with COVID-19, with some studies reporting an incidence of PTE ranging from 22% to 39%, the group noted. Cavagna and colleagues sought to evaluate CTPA findings of PTE in these patients through a study that included 109 hospitalized COVID-19 patients (average age, 64) who had CTPA for suspected pulmonary thromboembolism between March 20 and May 3. The authors assessed the CTPA findings, dividing patients into two groups defined by the presence or absence of PTE.
The authors found that 40.6% of patients had PTE and that in most patients, the condition manifested bilaterally or only on the right (90.2%), involved segmental (90.2%) or subsegmental (61%) arteries, and affected mainly lower lung lobes (73.2%).
Of the arteries with PTE, 67.6% showed a consolidation pattern; deep vein thrombosis was identified in only 12.2% of patients. The researchers did not find significant differences between patients with PTE and those without when it came to age, gender, symptoms, comorbidities, tumor history, use of respiratory supports, or the presence of deep vein thrombosis, but they did find statistically significant differences between the groups regarding CT lesion scores and D-dimer, lactate dehydrogenase, and C-reactive protein values: Those with higher scores had more severe disease.
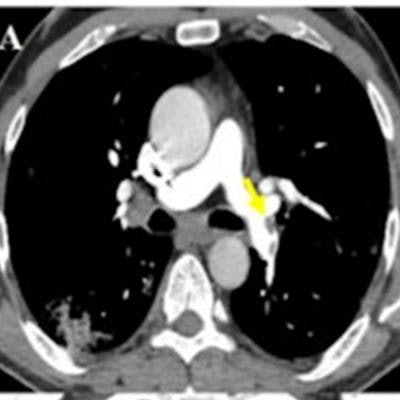
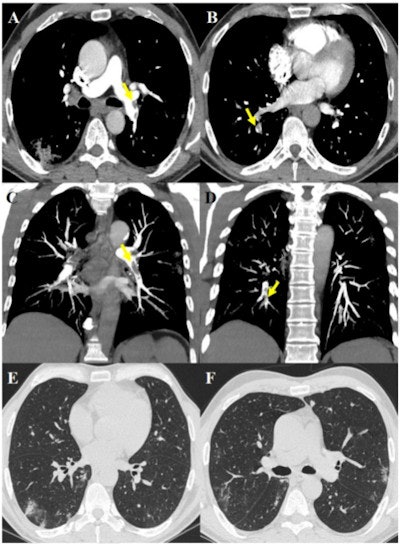 63-year-old male after 17 days of hospitalization without respiratory support and sudden increase of D-dimer value. The images show pulmonary thromboembolism in the lobar arteries for the left lower lobe (yellow arrow, A) and in the segmental arteries for the right lower lobe (yellow arrows, B), confirmed by maximum intensity projection reconstructions (yellow arrows, C and D). Lung parenchyma is characterized by some peripheral subpleural bilateral ground-glass opacities and consolidations (E, F). Images and caption courtesy of the RSNA.
63-year-old male after 17 days of hospitalization without respiratory support and sudden increase of D-dimer value. The images show pulmonary thromboembolism in the lobar arteries for the left lower lobe (yellow arrow, A) and in the segmental arteries for the right lower lobe (yellow arrows, B), confirmed by maximum intensity projection reconstructions (yellow arrows, C and D). Lung parenchyma is characterized by some peripheral subpleural bilateral ground-glass opacities and consolidations (E, F). Images and caption courtesy of the RSNA.The study results may suggest that proactive anticoagulant treatment could be effective for patients with COVID-19, the investigators wrote.
"[Our findings] may support the hypothesis that filling defects seen in pulmonary artery branches could be related to thrombosis rather than thromboembolic phenomena in COVID-19," they wrote. "This could have clinical implications as this hypothesis could support the indication of anticoagulant therapy as part of the first line therapeutic approach, regardless of traditional risk factors for deep vein thrombosis."
But more research is necessary, according to Cavagna and colleagues.
"Further studies are still needed to settle the discussion between the thrombosis versus embolic hypothesis, as well as to evaluate the prognostic role of PTE in these patients and to evaluate the management of anticoagulants," they concluded.





















