Scanning acute ischemic stroke patients with CT angiography (CTA) helps determine if they have COVID-19 faster than waiting for results from a nasal swab, say researchers in a study published October 29 in Stroke. The findings add to the debate over the best time to use CT during COVID-19.
The research team, led by Dr. Charles Esenwa of Montefiore Medical Center in New York City, examined lung findings in patients who were positive and negative for COVID-19 to determine if CTA could accurately detect the virus. They found, yes, it could, with a 92% accuracy (Stroke, October 29, 2020).
"Because this analysis is much faster and at no extra cost, we hope it could be incorporated as a rapid diagnosis tool for patients with acute stroke," Esenwa said in an accompanying press release. "In addition, accurately diagnosing COVID-19 within hours, rather than the sometimes days wait-time to receive the results from nasal swab tests, could help protect both patients and medical professionals."
Why use CTA for COVID-19 assessment?
CTA of the head and neck is used in emergency situations, such as for acute ischemic stroke patients, to evaluate large-vessel occlusion; scans typically include visualizing lung apices. This visualization provides an opportunity to screen for peripheral ground-glass and consolidative opacities suggestive of COVID-19-related pneumonia.
And although rapid COVID-19 tests are hitting the market, the most common test in use is still reverse transcription polymerase chain reaction (RT-PCR), which has a turnaround time of a day or more. Could CTA help not only identify large-vessel occlusion but also COVID-19? That's what the researchers sought to determine.
In their respective analysis, they included 57 patients from three hospitals in the Bronx, New York City, from March 1 to April 30. There were 30 patients in the COVID-19-positive group and 27 in the negative group. The patients received CTA scans on a 64-slice CT scanner (LightSpeed VCT, GE Healthcare) within 24 hours of hospitalization for acute ischemic stroke.
Esenwa and his team evaluated the lung apices for signs of COVID-19 pneumonia using CTA scans alone as well as in combination with patient-reported symptoms, such as cough and/or shortness of breath.
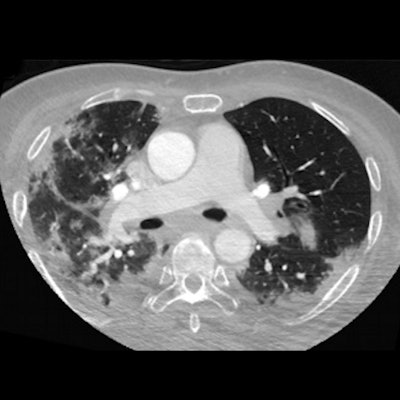
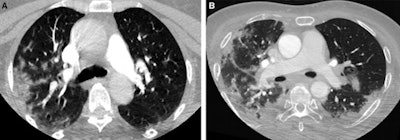 Axial CT images from head and neck CT angiography demonstrate (A) predominantly unilateral peripheral patchy ground-glass opacities, highly suspicious for COVID-19 pneumonia and (B) bilateral and multifocal, predominantly peripheral ground-glass opacities, with subpleural consolidations abutting the visceral pleura, with additional linear opacities, very highly suspicious for COVID-19 pneumonia. Images courtesy of Stroke.
Axial CT images from head and neck CT angiography demonstrate (A) predominantly unilateral peripheral patchy ground-glass opacities, highly suspicious for COVID-19 pneumonia and (B) bilateral and multifocal, predominantly peripheral ground-glass opacities, with subpleural consolidations abutting the visceral pleura, with additional linear opacities, very highly suspicious for COVID-19 pneumonia. Images courtesy of Stroke.They found 20 (67%) patients in the COVID-19-positive group and two (7%) in the COVID-19-negative group with lung findings highly or very highly suspicious for COVID-19 pneumonia.
Other findings are included in the chart below:
| CTA diagnosis of COVID-19 in stroke patients | |||||
| Sensitivity | Specificity | Positive predictive value (PPV) | Negative predictive value (NPV) | Accuracy | |
| CTA alone | 67% | 93% | 19% | 99% | 92% |
When CTA was combined with self-reported clinical symptoms of cough or dyspnea, sensitivity of apical lung assessment improved to 83%, the researchers reported. In contrast, the sensitivity of a one-time RT-PCR for SARS-CoV-2 has been reported to be 72% for sputum and 63% for nasal swab, according to a study by Wang et al published in the Journal of the American Medical Association (March 11, 2020).
"Screening questionnaires alone are often inaccurate because of the absence of symptoms or the patient is unable to speak because they are suffering from an acute stroke," Esenwa said in the press release. "Early diagnosis via CT scans has helped our center protect other patients and staff through early isolation, and it has also allowed us to start early supportive care for those suspected of having stroke that are COVID-19 positive."
However, when apical lung findings are absent, that cannot be the sole criteria used for screening COVID-19 in patients with acute ischemic stroke who require mechanical thrombectomy or rapid triaging. Instead, Esenwa and colleagues recommend an acute stroke algorithm that incorporates COVID-19 screening questions, apical lung assessment, and systematic SARS-CoV-2 RT-PCR testing to rapidly identify patients.