The number of cases of eosinophilic esophagitis, a chronic inflammatory disorder of the esophagus, is rising in pediatric populations. However, endoscopy and pathological testing should remain the primary means of diagnosing the disease, not esophagrams, according to radiologists at Cincinnati Children's Hospital Medical Center.
Gastroenterologists from the pediatric hospital estimate that one in 10,000 children is diagnosed with eosinophilic esophagitis (EE). The condition was not identified until the late 1980s, and its prevalence has increased dramatically, a factor attributed to both increasing awareness by clinicians and environmental factors.
A multidisciplinary team conducted a study to determine the utility of fluoroscopy exams (esophagrams) as a primary diagnostic tool for EE and to evaluate the type and frequency of fluoroscopic findings of children diagnosed with EE. They followed this research with a study to determine if EE was the most common cause of children admitted to the hospital's emergency department with food impaction. Dr. Lincoln Diniz, a radiology fellow, presented their results at the RSNA annual meeting, held earlier this month in Chicago.
Dysphagia symptoms
Pediatric patients suspected of having eosinophilic esophagitis have symptoms of dysphagia, or difficulty in swallowing, as well as vomiting, atypical chest pain, and/or food sticking in the throat and food impaction. The gastrointestinal tract contains increased numbers of eosinophils, a white blood cell, or other granulocytes.
The cause of the condition is unknown, but its increasing prevalence is similar to increases in asthma, eczema, allergic rhinitis, and other atopic diseases. Clinicians believe the disease is caused by food allergens and aeroallergens, and its documented occurrence in families suggests a genetic predisposition.
The research team, led by Dr. Alexander Towbin, assistant professor of radiology and assistant director of thoracoabdominal imaging, used a gastrointestinal-specific clinical database to identify all patients diagnosed by esophageal biopsy with EE between January 2000 and August 2008 at Cincinnati Children's. The hospital's PACS was used to identify the number of these patients who had an upper GI study or esophagram performed. The majority of esophagrams were single-contrast studies.
In all, 133 patients were identified. They ranged in age from 7 months to 21 years, with a mean age of 8 years, and 71% were boys.
Two radiologists reviewed each of the images and reports for a total of 151 studies. They evaluated each study for the presence or absence of esophageal strictures, rings, mucosal irregularity, irregular contractions, or impacted food. They reviewed the radiology reports to ensure a contemporaneous diagnosis of gastroesophageal reflux or esophageal dysmotility, Diniz said.
Seventy-one patients, or 53% of the total, were normal. Diniz attributed the lack of imaging findings to deep infiltration, mild inflammation, or mucosal findings that could not be identified on a single contrast study.
Twenty percent of the patients had gastroesophageal reflux, and 14% had irregular contractions. Eleven patients were diagnosed with strictures, three in the midesophagus and eight in the distal esophagus. Nine patients were identified with dysmotility, seven with mucosal irregularities, six with rings, and three with filling defects.
Incidental findings included paraesophageal hernia, hiatal hernia, contained leaks, and distal esophageal diverticula.
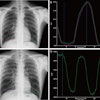
 |
| Single-contrast esophagrams in five different patients with eosinophilic esophagitis show the different findings of this disorder. Left to right: gastroesophageal reflux, midesophageal stricture, a ringed esophagus, dysmotility, and an impacted food bolus. Image courtesy of Dr. Alexander Towbin, Cincinnati Children's Hospital Medical Center. |
The study found that the utility of esophagrams was limited in this patient population. Although approximately 50% of the patients had at least one esophageal finding at fluoroscopy, no one finding occurred with enough frequency to reliably suggest a diagnosis, they said.
"Our hypothesis before we began this investigation was that upper GI exams are not useful studies in the primary diagnosis of EE. This proved to be true," Towbin told AuntMinnie.com in a subsequent telephone interview. "In our opinion, an esophagram is not a useful method to diagnose eosinophilic esophagitis, although it can be used to answer a specific question, such as if a stricture is present."
In this situation, Towbin advised that the radiologist should be informed of the potential findings of EE.
"If the clinical question is 'Does this patient have EE?' an esophagram should not be ordered. The child should be spared the radiation dose exposure from this examination," Towbin emphasized.
EE: Main cause of food impaction
In the related study presented at RSNA by the Cincinnati Children's team, they evaluated the causes of food impaction in children, as well as the percentage of children with food impaction who also have EE.
Food impaction requiring emergency care intervention is usually attributed to either an esophageal stricture caused by prior esophageal atresia with tracheoesophageal fistula repair, or to eosinophilic esophagitis. In children with EE, infiltration of the esophagus with eosinophils leads to edema and inflammation with possible fibrosis over time. Eosinophilic infiltration can alter the structural integrity, luminal patency, and motility of the esophagus.
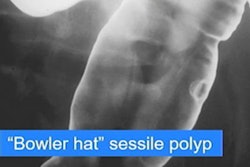
To determine the frequency of children presenting with food impaction who have confirmed EE from endoscopy and pathology reports, the researchers conducted a search of all upper GI and esophagram reports dictated between 1993 and March 2009 contained in the hospital's electronic medical record database. Search terms included "impacted food," "food impaction," and "filling defect."
The researchers identified 46 patients with filling defects from a review of 475 patient records. The patients ranged in age from 1 month to 31 years, with a mean age of 9.5 years; 61% of the patients were male.
Half of these patients, or 23 children (16 male, seven female), had biopsy-proven EE. Eleven children, or 24% of the group that had a filling defect, had a history of prior esophageal atresia with tracheoesophageal fistula repair. Three patients had both conditions. Four patients had prior Nissen fundoplication, a surgical procedure to treat gastroesophageal reflux disease and hiatus hernia. Nine patients had not been biopsied or had no identifiable cause of food impaction.
The high percentage of food impaction in children with EE is probably due to the structural and functional alterations that occur in the esophagus from prolonged inflammations, Diniz said.
By Cynthia E. Keen
AuntMinnie.com staff writer
December 31, 2009
Related Reading
Patient position tips for a premium UGI series, April 17, 2002
Copyright © 2009 AuntMinnie.com