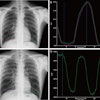
A new Chinese study questions the assumption that striving for the highest possible image quality is always the best approach. Researchers developed an x-ray optimization strategy that cuts the dose of digital radiography (DR) substantially by adjusting dose levels based on the type of exam being conducted.
The imaging protocols developed by Dr. Menglong Zhang, from Shandong Medical Imaging Research Institute, and colleagues tailor equipment settings to the clinical task at hand, using manufacturer-provided exposure index values as a guide to reducing dose.
Such task-dependent settings could be a way to combat DR "dose creep," or the tendency of radiologic technologists to ratchet up tube current and other DR settings to optimize image quality at the cost of high radiation exposure. The study was published in the September issue of Health Physics (Vol. 103:3, pp. 235-240).
Battling dose creep
Medical physicists have battled dose creep since DR's introduction. For technologists, underexposed DR images will draw criticism from radiologists and orders to repeat studies because of poor image quality. Overexposed DR, on the other hand, can be corrected to produce a high-quality image, though the patient is exposed to a higher-than-necessary level of radiation. Doses tend to creep higher as technologists strive to avoid complaints.
Radiologists have been attempting to apply diagnostic reference levels to medical imaging since at least the early 1990s, noted Mayo Clinic medical physicist Cynthia McCollough, PhD, in a 2010 analysis for the Image Wisely dose reduction program. A system developed by the International Commission on Radiological Protection (ICRP) was introduced in 1996 and intended to supplement professional judgment rather than provide a dividing line between good and bad medicine, she wrote.
In 2009, the American Association of Physicists in Medicine (AAPM) concluded that a clear indicator of exposure is needed to prevent dose creep, Zhang and colleagues wrote. Though limited to chest radiography, Zhang's study suggests that an exposure index (EI) can play that role.
The framework of the study is based on a three-level classification system, developed by the authors, for matching the need for high, medium, and low image quality to specific chest applications. Their format is similar to one developed by North American and European medical physicists for the Dose and Image Quality in Digital Imaging and Interventional Radiology (DIMOND) project (Radiation Protection Dosimetry, December 2005, Vol. 117:1-3, pp. 143-147).
In the system developed by Zhang and colleagues, the three clinical task types are as follows:
- Type I: High image quality for primary bone and lung tumors; rib, clavicle, or thoracic vertebrae fractures; and suspected pneumothorax
- Type II: Medium image quality for chronic back pain with no indication of infection or neoplasm; newly diagnosed pneumonia, tuberculosis, and pneumoconiosis; pleural effusion detection; and mediastinum tumors
- Type III: Low image quality for observation of size and shape of the heart; thoracic scoliosis; metallic foreign bodies in the esophagus; internal fixation of clavicle fracture, thoracic surgery metal implants, pacemaker implantation, and metal valve replacement (review); and pneumonia, tuberculosis, and atelectasis (follow-up)
A phantom study was first performed. It established an exposure factor of 3.9 mAs, with an exposure control factor (ECF) of -1 and EI of 1,550 as optimal for high-quality DR imaging. Zhang and colleagues chose 2.0 mAs and 1.0 mAs as optimal for medium and low image quality, respectively, based on recommendations from the ICRP and International Organization for Standardization. ICRP calls for reducing dose by half (50%) for clinical class type II procedures and half again (25%) for level III procedures.
Proposed standards for optimized DR for high-, medium-, and low-quality imaging are described in the table below.
Optimum DR exposure by clinical task type
|
||||||||||||||||||||||||||||||||||||
| Source: Zhang et al in Health Physics |
Clinical study
The standards were tested on 60 consecutive patients of similar size and body weight. Half were randomly selected for routine DR studies using exposure factors determined by the DR system's automatic exposure control and an ECF setting of 0. The other 30 patients were imaged using task-dependent exposure factors that produced optimal exposure reading in the phantom study.
The results indicate that the task-dependent approach to setting DR exposures provided adequate image quality, according to results from three experienced radiologists, while substantially reducing patient radiation exposure.
The mean entrance surface dose for the routine group was 0.168 mGy, compared with 0.092 mGy for the task-dependent group (p < 0.0001). The mean detector dose for the routine group was 3.14 µGy, compared with 1.41 µGy for the task-dependent group, a difference that reached the same high level of statistical significance.
The entrance surface dose of the task-dependent group was approximately two times lower than that of the routine group for the medium image quality category and four times lower for the low image quality category.
Dose optimization is easier to perform on hospitalized patients than outpatients, the authors noted. This is because more relevant clinical information is available to rank inpatients' appropriate imaging level compared to outpatients, especially for first-time visitors.
Zhang and colleagues also warned against becoming inflexible when applying exposure indexes. "An experienced technician should always set suitable EI values for the specific imaging tasks based on the patient's condition and the status of the equipment that he or she operates," they wrote.
Though image quality can vary, the ultimate standard of radiological practice does not change, the authors stressed.
"Patients and clinicians always expect radiologists to refer all abnormalities to them, or radiologists will be held accountable for misdiagnosis," they wrote.