Endovascular thrombectomy (EVT) may be an underused procedure in patients who experience stroke during or after cardiac surgery, according to a study published January 29 in JAMA Neurology.
In an analysis of patient records, EVT was half as likely to be used to treat stroke patients undergoing cardiac interventions than those not undergoing interventions. This is despite better outcomes for patients who undergo EVT, noted lead author Adam de Havenon, MD, of Yale University in New Haven, CT, and colleagues.
“Among individuals with a cardiac intervention, receiving EVT was associated with a twofold higher chance of discharge home,” the group wrote.
Cardiac surgery is associated with a risk of ischemic stroke during or after the surgery in 1% to 2% of patients, the authors explained. Many of these patients are not eligible for intravenous thrombolytic treatment -- the use of clot-dissolving drugs -- because of the risk of postsurgical hemorrhage, they added.
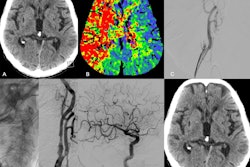
Alternatively, EVT is a minimally invasive image-guided surgical procedure that can be used to dissolve blood clots in these patients, and thus restore blood flow to prevent further brain damage. Yet data remain sparse on the use of EVT in these settings, the group noted.
To bridge this knowledge gap, the team analyzed procedure rates from 4,888 U.S. hospitals between 2016 and 2020. The identified 634,407 stroke patients (mean age, 69.8 years old; 50.2% men, 49.8% women), a total of 12,093 of whom had undergone a cardiac intervention.
According to the results, EVT was performed in 194 patients (1.6%) of these patients compared with being used in 23,660 patients (3.8%) who had not undergone a cardiac intervention, the group wrote. In addition, further analysis revealed that among individuals with a cardiac intervention, receiving EVT was associated with a twofold higher chance of discharge home, the team added.
“In this study, patients hospitalized with ischemic stroke and cardiac intervention may be less than half as likely to receive EVT as those without cardiac intervention,” the group wrote.
Ultimately, the lower rates of EVT after cardiac intervention seen in the study could be explained by multiple factors: delays in diagnosis, clinician reluctance due to perceived higher procedural risk, or patients being ineligible, the researchers suggested.
They noted that additional studies are needed to explore these issues.
“Given the known benefit of EVT, there is a need to better understand the reasons for lower rates of EVT in this patient population,” the researchers concluded.
The full article is available here.