
According to the poet Alfred Lord Tennyson, it is the sights, sounds, and smells of a season that puts the male of the species in a frisky mood. "In the spring, a young man's fancy lightly turns to thoughts of love," Tennyson cooed in "Locksley Hall."
But put a racy image in front of a young man, and his "fancy" will bolt upright and pay very close attention: The results of a recent functional MRI (fMRI) study reveal that men show greater neurological activation than women when viewing sexual stimuli -- even if women report greater arousal.
Young men aren't the only ones having fun. In an effort to shed light on the mysteries of female sexuality, a group from the University of Washington in Seattle used serial MRI, along with a new contrast agent, to study female sexual arousal response.
Of course, it's not really the youngsters who need to have their sexual habits studied -- as the population grays and grows older, sexual dysfunction will become a more pressing issue.
According to sociological research out of the University of Chicago, men -- especially those 75 and over -- are more likely to contend with physical ailments, such as erectile dysfunction. Women, on the other hand, are more likely to suffer from a lack of interest than ability (2002 International Society for the Study of Women's Sexual Health conference, Vancouver).
Recently, cardiologists found that middle-aged men with certain risk factors -- obesity or high cholesterol, for example -- are apt to develop erectile dysfunction down the road (Journal of the American College of Cardiology online, April 21, 2004).
In women, use of the ubiquitous antidepressant Prozac (fluoxetine) could affect their ability to achieve sexual climax, according to a report issued by the U.S. National Toxicology Program (ReutersHealth, April 27, 2004).
Sexual dysfunction can also be caused by diseases such as diabetes mellitus, coronary artery disease, atherosclerosis, temporal lobe epilepsy, or trauma (spinal cord injury). Diagnostic procedures for studying sexual dysfunction and the relationship to these issues are currently scarce, which is where imaging may come to the rescue (Der Urologe A, October 2003, Vol. 42:10, pp.1317-1321).
Here's a peek into how imaging is tuning us in to what turns us on.
Am I hot or not?
During its heyday, the Web site mentioned above got its fair share of attention. Visitors were asked to rate pictures of strangers and determine how attractive they were. A group from Emory University in Atlanta took a similar, if decidedly more sophisticated, approach for their study on gender-based response to sexual imagery.
"The amygdala response to appetitive visual sexual stimuli were not solely determined by arousal, but instead were strongly influenced by the sex of the viewer," wrote Dr. Stephan Hamann in Nature Neuroscience (April 2004, Vol. 7:4, pp. 411-416).
Hamann and co-authors are from the university's department of psychology, as well as the Yerkes National Primate Research Center at Emory.
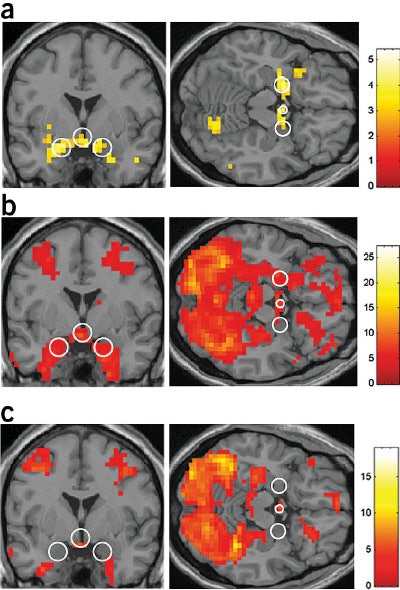 |
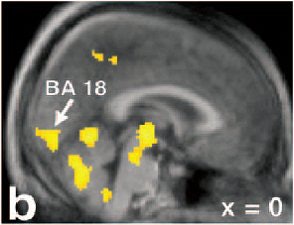
| Regional activation maps. Activation contrast for the couples stimuli versus fixation (a-c, above) and the couples stimuli versus neutral contrast (d-f, below). Left, coronal image (a) showing greater bilateral amygdala and hypothalamic activations for males versus females for the couples versus fixation contrast. Couples versus fixation contrast for males, at the same coronal and axial views (b). The same contrast and views for females (c). |
For this study, 28 young adult, heterosexual subjects, evenly split between male and female, underwent MR scans on a 1.5-tesla Intera scanner (Philips Medical Systems, Andover, MA). First, a T1-weighted anatomical scan was done. The subjects then underwent whole-brain functional runs in order to gather blood oxygen level-dependent (BOLD) effects. The imaging protocol included echo-planar imaging and gradient recalled echo. Twenty-five 5-mm axial slices were obtained.
The data were analyzed with SPM99 software (Wellcome Department of Cognitive Neurology, University College London, U.K). The amygdala and hypothalamus were defined as the regions of interest (ROI).
During the two 15-minute imaging runs, the subjects alternately viewed pictures of four types of stimuli:
- Heterosexual couples engaged in explicit sexual activity.
- Attractive opposite-sex nudes in modeling poses.
- Partially or fully clothed men and women in pleasant social interaction (e.g. dancing, wedding).
- Neutral image of a visual fixation cross.
The authors calculated the average fMRI signal change relative to the fixation baseline across all stimulus conditions.
According to the results, men had greater neural responses in the bilateral amygdala and hypothalamus than did women in response to images of the couples engaged in sexual activity (p<0.001). Those same images also produced greater activations in the left amygdala, and marginally greater activations in the right amygdala and hypothalamus, in men than in women (p<0.001). Additionally, men showed greater focal differential activations at a lower statistical threshold in both sides of the amygdala (p<0.005), as well as in the hypothalamus, bilateral posterior thalamus, and left hippocampus.
Finally, there was some overlap in response between the sexes, most notably in the bilateral parieto-temporal region (visual processing, somatosensory function) and the anterior cingulate (emotion, sexual motivation).
 |
| Left, coronal image (d) showing greater bilateral amygdala activations for males versus females for the couples versus neutral stimuli contrast within those regions showing greater activity for males versus females. Couples versus neutral stimuli contrast for males (e), at the same coronal and axial views. The same contrast and views for females (f), showing an absence of differential activity in the ROIs. Figure 2 from Nature Neuroscience, Vol.7, pp. 411 to 416, "Men and women differ in amygdala response to visual sexual stimuli" by Stephan Hamann, Rebecca A Herman, Carla L Nolan, Kim Wallen , et al. |
"Notably, in no region did females show significantly greater activation than males...the greater amygdala activation in males observed here may in part reflect a greater appetitive incentive value of visual sexual stimuli...," Hamann and colleagues noted.
The results could eventually aid understanding of disorders such as hyperactive or hypoactive sexual arousal and desire, Hamann said in an e-mail interview.
"For example, males appear to have a greater vulnerability to becoming 'addicted' to Internet pornography sites, sometimes spending large amounts of time and money, negatively affecting other social relationships," he said. "This greater propensity to respond in this way to sexually explicit images may be relevant to the sex difference we found."
The amorous amygdala, the come-hither cerebellum
It's no surprise that Hamann's results jibe with those of earlier studies concluding that the sex drive hooked up with the portions of the brain generally associated with rewards. Figuring out the neurotransmitters involved in a healthy arousal response can go a long way toward helping people who must contend with non-age-related sexual dysfunction.
Dr. Gert Holstege from University Hospital in Groningen, the Netherlands used PET to measure regional blood flow (rCBF) and brain activation during human male ejaculation.
"Patients suffering from brain disease such as cerebrovascular accidents or Parkinson's disease experience sexual dysfunction...the design of the present PET study provides the time-scale resolution necessary to identify brain regions that are specifically activated during ejaculation and orgasm," wrote Holstege, who is from the department of anatomy and embryology. Holstege's co-authors include Dr. Anne Paans from the PET Centre and radiologist Dr. Linda Meiners (Journal of Neuroscience, October 8, 2003, Vol. 23:27, pp. 9185-9193).
For this study, 11 heterosexual male volunteers underwent PET imaging on an ECAT Exact HR+ (CTI PET Systems, Knoxville, TN; Siemens Medical Solutions, Malvern, PA), 30 seconds after the injection of 500 MBq of 15O in saline. Data was collected for two minutes.
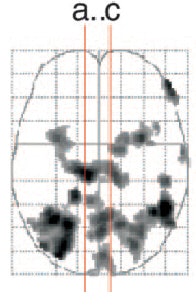 |
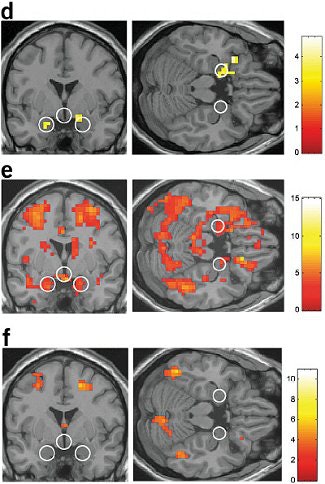
| Sagittal view of the activations in midline cortical structures, the mesodiencephalic transition zone, and the cerebellum. Increased rCBF is represented in sagittal sections, of which the location is indicated by the red lines on the glass brain (above). |
The volunteers were asked to perform the following tasks twice: rest, erection, sexual stimulation/manual manipulation by a female partner, and ejaculation. The participants were asked to ejaculate within the first 50 seconds after the arrival of the tracer to the brain; eight subjects were successful.
The authors reported the strongest activation at the mesodiencephalic junction, including the ventral tegmental area (VTA), the subparafascicular nuclear, and the medial and ventral thalamus. Increased rCBF was also found in the anterior nucleus of the right thalamus and in the inferior temporal cortex.
  |
Activations are superimposed on the averaged MRI of the volunteers. Activation in the secondary visual cortex (b, BA 18) and the posterior cingulate/precuneus (c, BA 23/31) can be found. Note in sections a-c that the activation in the mesodiencephalic transition zone (mes-di) extends from the rostral midbrain into the ventral parts of the caudal thalamus x = 12 mm left to the intercommissural line. Holstege G, Georgiadis JR, Paans AM, Meiners LC, van der Graaf FH, Reinders AA, "Brain activation during human male ejaculation," J Neurosci 2003 Oct 8:23(27):9185-93. Copyright 2003 by the Society for Neuroscience.
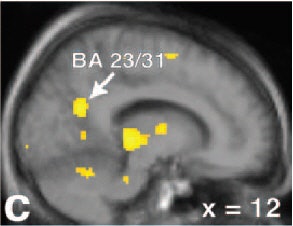 |
Finally, "remarkably strong rCBF increases were observed in the cerebellum," they said. "These findings corroborate the recent notion that the cerebellum plays an important role in emotional processing."
For example, the main complaint of people who sustain spinal cord injuries is the inability to maintain a normal sex life rather than the inability to walk, Holstege wrote. The results of this PET study may show just how strongly reinforcing, or rewarding, sexual activity is in humans.
As counterintuitive as it may seem, some physical limitations or changes may actually enhance the sex-driven rewards. Australian investigators studied people with temporal lobe epilepsy (TLE) whose condition improved their sex lives.
Dr. David Reutens from the University of Melbourne and the Epilepsy Research Institute explored the relationship between the amygdala and sex drive in TLE patients before and after surgical resection.
"We tested the hypothesis that there are differences in preoperative amygdalar volume between groups of patients who report a postoperative sexual increase, decrease, or no change," they wrote (Annals of Neurology, January 2004, Vol. 55:1, pp. 87-96).
Using MRI, they assessed 45 patients who had undergone a range of surgical procedures, including anterior temporal lobectomies, limited temporal neocortical resections, and parahippocampal resections. The patients also completed a questionnaire on postsurgical sexual outcomes.
The subjects underwent scanning on either a 1.5-tesla Magnetom 63 (Siemens Medical Solutions, Erlangen, Germany) or a Signa Horizon EchoSpeed (GE Healthcare, Waukesha, WI). According to the results, patients who reported a postoperative sexual increase (a jump in sexual drive, activity, or masturbation) also had a significantly larger contralateral amygdala. The mean contralateral amygdalar volume in the sexual increase group was greater as well.
"The postoperative sexual increase described by our patients primarily consists of an increase in sex drive without indiscriminate sexual behavior," the group reported. "These findings are consistent with evidence from previous research...supporting a role for the amygdala...in the processing of sexual incentives."
Of course, there were some differences along gender lines. Fifty-seven percent of the men (12 of 21) reported a sexual increase postresection compared with 43% of the women (9 of 21). Conversely, 60% of the women reported sexual decrease (6 of 10) versus 40% of the men.
Girl power
For older women who suffer from sexual dysfunction, the culprit is generally a decline in estrogen at the time of menopause. Physical ailments such as hot flashes and thinning of the vaginal wall can even make sex painful. In younger women, clinical depression and anxiety can lead to a diminished interest in sex, or it can occur as a byproduct of psychotropic drugs. And unfortunately, Viagra-type products have proved ineffectual in the majority of women.
But the mechanics of female arousal are still a murky area. For the most part, studying arousal in this population has required invasive techniques such as vaginal photoplesthysmography (using a probe that measures blood flow). Obtaining information on female sexual dysfunction is hardly a wham-bam-thank-you-ma'am undertaking.
"(Female sexual dysfunction) is poorly understood for several reasons. It has not been studied as long or as in-depth as male dysfunction...women seem to be more complex than men. It is not just (about) blood flow," explained Dr. Kenneth Maravilla in an e-mail to AuntMinnie.com.
Maravilla, from the department of radiology at the University of Washington in Seattle, has spearheaded the use of MR imaging for studying female sexual function and dysfunction.
"An important part of research is to establish a definitive, reproducible method to allow objective monitoring and quantification of (female sexual arousal response)," Maravilla and co-authors wrote in their latest article (Journal of Magnetic Resonance Imaging, August 2003, Vol. 18:2, pp. 216-224).
They built on research that they originally published in 2002, using dynamic MRI in combination with MS-325 (Epix Medical, Cambridge, MA), a gadolinium-based blood pool agent (Radiology, December 2002, Vol. 225:3, pp. 791-799).
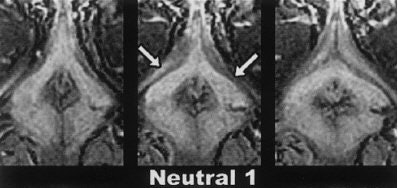 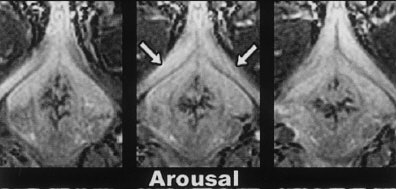 |
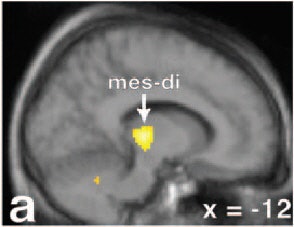
Three contiguous transverse 2-mm MR image sections, obtained in the same subject at three different times. The top images were obtained while the subject viewed neutral video material; the middle images, while the subject was aroused by erotic video material; and the bottom images, while the subject viewed the second neutral video after having been aroused by the erotic video presentation. Note the change in size of the crura of the clitoris (arrows) in response to each video segment. Figure 4, Deliganis AV, Maravilla KR, Helman JR, et al, "Female genitalia: dynamic MR imaging with use of MS-325 -- Initial experiences evaluating female sexual response." Radiology 2002; 225:791-799.
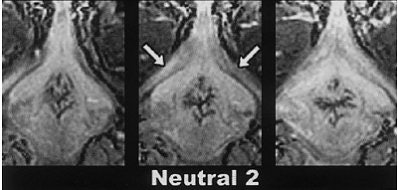 |
For the most recent study, nine healthy heterosexual women (six premenopausal, three postmenopausal), ages 22-57, were enrolled. The subjects were scanned on 1.5-tesla Signa Horizon EchoSpeed during two separate MR sessions, separated by a 45-minute rest interval. A single injection of MS-325 (0.05 mmol/kg) was given about three minutes before the first session.
"MS-325 binds reversibly to albumin, prolonging its intravascular half-life," the authors explained. "This results in excellent visualization of blood vessels and intravascular spaces for an extended length of time."
During each imaging run, the subjects were shown a video of 15 minutes of neutral material, 15 minutes of sexually explicit material, and then another quarter of an hour's worth of neutral footage.
Serial images of the external genitalia were obtained using a T1-weighted, fast 3D spoiled gradient-echo sequence in the axial plane. Sagittal and coronal localizer images in the area of interest were also obtained. The regions of interest (ROI) were defined as the right crus of the clitoris and within the femoral vein.
First, the group reported that a qualitative visual evaluation of the post-injection MS-325 images showed excellent enhancement of genital structures during both sessions, including increases in clitoral signal intensity and volume.
"Across all subjects, the average percent change in signal intensity from baseline to arousal increased approximately 90% in session 1 and 32% in session 2," Maravilla and colleagues reported. "For all subjects, the combined percent change of both sessions was over 108%, with a range between 16% and 260%." In premenopausal women, the average percent change in clitoral volume measured 121%; in postmenopausal women, it was 81%.
The group concluded that MRI with MS-325 "may prove to be an excellent method for monitoring therapeutic treatments in women with sexual arousal disorder."
Sex & the sildenafil citrate
"The recent enormous success of sexual potency-increasing drugs is a reflection of the magnitude of problems in the field of sexual health," Holstege commented. Certainly no review of sexual imaging would be satisfactory without a mention of Viagra or its offspring, Levitra and Cialis.
Unfortunately, there isn't a lot to say at this point. The majority of imaging-related studies have focused on the side effects of these medications rather than their direct effects on sexual dysfunction, such as studies that have touted echocardiography for assessing coronary artery disease or ultrasound for tracking vascular congestion and visual decline in Viagra users (International Journal of Cardiology, August 2003, Vol. 90:2-3, pp. 291-295; Ophthalmologica, November-December 2002, Vol. 216:6, pp. 455-458).
But imaging studies have value in helping us understand the brain mechanisms involved in sexual behavior, Hamann pointed out, and how these performance-enhancing drugs affect the brain.
On a broader social level, imaging-based studies can also offer insight into what drives human lust and how that drive can be applied to life in general. A host of ongoing studies have suggested that sexual activity can protect against heart disease, boost immunity levels, and lower cancer risk (Time, January 19, 2004).
Sex may even allow Tennyson's young man to see spring many times over: A recent study of 3,500 Scottish males found a link between frequent intercourse and a longer lifespan.
By Shalmali PalAuntMinnie.com staff writer
April 28, 2004
Front and above: Eternal lovers from a temple panel at Khajuraho, Madhya Pradesh, India. Copyright © 1996-2002. Kamat's Potpourri. All Rights Reserved.
Related Reading
Ejaculation does not raise prostate cancer risk, April 7, 2004
Epix gets U.S. patent for MS-325, January 13, 2004
Viagra helps men with erectile dysfunction after radiation therapy, November 13, 2003
Same parts of brain say "ouch" when hurt physically or emotionally, October 24, 2003
Ultrasound, topical PGE-1 might help "objectify" female sexual dysfunction, January 22, 2003
Sex in an MRI provides new 'phallatious' findings, December 31, 1999
Copyright © 2004 AuntMinnie.com



















