Asbestos-related deaths in the U.S. have skyrocketed since the late 1960s, according to Centers for Disease Control and Prevention (CDC) statistics. Asbestos-induced conditions have become a bigger killer than silicosis and black lung, and are considered the deadliest of all work-related respiratory illnesses.
Nearly 1,500 people died from an asbestos-induced condition in 2000, and that number is expected to climb, particularly because of the tremendous lag time, up to 45 years, between initial exposure to asbestos fibers and death (Reuters Health, July 22, 2004).
It's a safe bet that more instances of asbestos-induced disease -- including pneumoconioses and mesothelioma -- could mean more lawsuits and, as a result, more chest x-rays for certified B readers to sign off. But will x-ray continue as the modality of choice for deciding these cases, especially given the plethora of other modalities that might do a better job? The jury is still out.
Inadequate x-ray?
The intentions and abilities of B readers aside, how good is x-ray at identifying asbestosis or other asbestos-induced disease? So-so, but many restrictions on how x-rays are read can be pinned on the criteria of the 24-year-old International Labour Organization (ILO) classification system.
The main asbestos-induced conditions and diseases are pleural effusion, pleural plaque, diffuse pleural thickening, asbestosis, bronchogenic carcinoma, and malignant mesothelioma.
The ILO reporting system covers parenchymal and pleural abnormalities as seen on posteroanterior chest radiographs. However, it does not define pathologic entities, explained Dr. Huw Roach and colleagues from the University Hospital of Wales and other Welsh institutions in Cardiff, U.K.
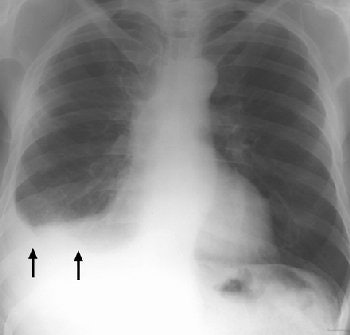 |
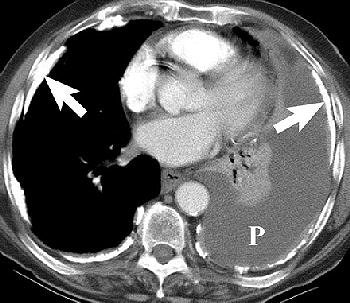
| Posteroanterior radiograph of an asbestos-exposed patient shows a right-sided pleural effusion (arrows). Figure 1, Roach HW, Davies GJ, "Asbestos: When the Dust Settles -- An Imaging Review of Asbestos-related Disease" (RadioGraphics 2002; 22: S167-S184). |
Moreover, the ILO system does not define a relationship between the level of abnormality and the level of compensation, or require that information from the chest x-ray be correlated with the person's occupation.
What does an x-ray reveal to a B reader looking at an asbestos-related case? The features of asbestosis on a chest radiograph include "ground-glass opacification, small nodular opacities, and 'shaggy' cardiac silhouette, and ill-defined diaphragmatic contours," wrote Roach's group in RadioGraphics (October 2002, Vol. 22: special issue, pp. S167-S184).
In terms of pleural plaques, the classic distribution on x-ray is seen on the posterolateral chest wall between the seventh and tenth ribs, the lateral chest wall between the sixth and ninth ribs, and the dome of the diaphragm, Roach stated. Pleural plaques are the most common manifestation of asbestos exposure.
In cases of malignant mesothelioma, the chest x-ray generally reveals an effusion, pleural thickening, and a contracted hemithorax.
Despite x-ray's ability to show these potential disease hot spots, it is simply not enough, according to Dr. Robert Ross from Baylor College of Medicine in Houston. Ross advocated against the chest radiograph being "used as the sole diagnostic toll as it will be wrong more often than it will be right" (Chest, September 2003, Vol. 124;3, pp.1220-1128).
Two of chest x-rays greatest failings are its lack of sensitivity and specificity, Ross argued, especially for minimal or mild disease.
"Is a radiographic finding of a mild increase in interstitial lung markings (ILO grade, 1/0 and 1/1) adequate by itself to diagnose asbestosis?" he said. "Many factors other than asbestos exposure can lead to a mildly abnormal chest radiographic finding." These factors -- including obesity, smoking, and exposure to other fibrogenic or nonfibrogenic dusts -- then call into question x-ray's specificity, Ross added.
What are the other imaging options? CT is certainly one, with its advocates touting its superiority to radiography. Other modalities, while useful, are better suited for asbestos-infected patients who have graduated to advanced disease stages.
CT instead of x-ray
The CT criteria for the diagnosis of asbestosis include subpleural curvilinear lines, subpleural density, parenchymal bands of fibrosis, and honeycombing.
The protocol for using CT to diagnose asbestosis was set by Dr. Gordon Gamsu and colleagues in a 1995 American Journal of Roentgenology article. Gamsu's group tested a semiquantitative scoring method, as well as a cumulative scoring method, for assessing the extent and severity of asbestos-related abnormalities seen with CT. They also compared the results of high-resolution CT to chest radiographs.
The patient population consisted of 24 live patients and six lungs obtained at autopsy; of the 30, 24 had asbestosis based on histopathology. The most prevalent CT abnormality in the asbestosis cases was interstitial lines (84%) followed by parenchymal bands (76%). The chest x-rays were classified by the ILO system.
 |
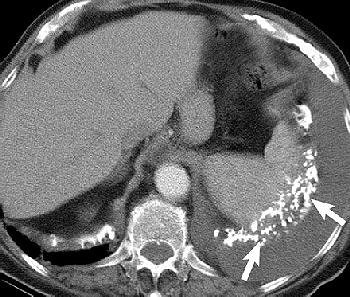
Pleural effusion in a 70-year-old man with a history of asbestos exposure and known left-sided MPM. Axial contrast-enhanced CT scans obtained at different levels show unilateral pleural effusion (P, above) with extensive calcified pleural plaques (arrows, below). Figure 1a-b, Wang ZJ, Reddy GP, et al, "Malignant Pleural Mesothelioma: Evaluation with CT, MR Imaging, and PET" (RadioGraphics 2004; 24: 105-119).
 |
According to the results, asbestosis was suggested in 64% of the cases based on the semiquantitative CT severity score. With the cumulative scoring method (based on multiple CT features), any one type of abnormality was found in 88 instances.
"However, to include only cases with asbestosis, three different abnormalities had to be present," they wrote. "The high-resolution CT scans were normal or near normal in five instances of asbestosis. Chest radiographs using the ILO classification predicted asbestosis with a less frequency than ... CT," (AJR, January 1995, Vol. 164:1, pp. 63-68).
Subsequent studies have indicated CT's value in fine-tuning asbestos-induced disease. Australian physicians tested various CT scoring systems for quantifying pleural thickening and correlated it with lung function. They developed a simple CT scoring system that evaluated disease at five anatomic levels, and found that it had "the ease of application and potential to aid in the accurate assessment of the lung parenchyma, which may be important in individuals exposed to asbestos" (Radiology, July 2001, Vol. 220:1, pp. 237-243).
Another study, out of Brazil, found that pairing CT imaging with pulmonary gas exchange impairment tests could clarify the degree of interstitial lung disease in workers exposed to asbestos (Radiology, July 2004, Vol. 232:1, pp. 66-74).
But CT is no magic modality in asbestos-induced cases, noted Dr. David Lynch in an AJR editorial. Although CT does seem more sensitive than x-ray, it cannot clarify that borderline between normal and abnormal findings. In addition, there is a phase of interstitial lung disease during which it is too focal or too mild to cause morphologic changes on CT (AJR, January 1995, Vol. 164:1, pp. 69-71).
Pathology on ultrasound
Sonography has no value in the detection of mesothelioma, but it can offer vital information for confirming and fine-tuning the initial diagnosis made with other modalities. Ultrasound is particularly useful for identifying disease changes to the chest wall, diaphragm, or upper chest aperture, explained Dr. Felix Herth from the department of pneumology at the Thoraxklinik in Heidelberg, Germany.
Herth recommended using a highly soluble transducer (5 MHz) to look at pathological findings in the chest wall of mesothelioma patients. In advance stages of the disease, tumor infiltration of the lung tissue will appear as echo-poor, oblong structures along the ventilated lung. Pleural metastases are also echo-poor, or moderately echo-close, and present as roundish, small, knotty, or laminar processes with irregular delimitation.
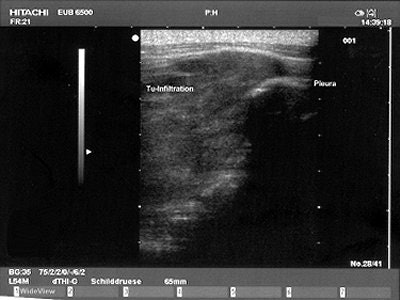 |
| A Brustwand echocardiogram depicting infiltrating carcinoma. |
"Pleural mesothelioma presents sonographically as an irregularly limited, echo-poor, knotty, or planar widening along the pleura," Herth wrote in Lung Cancer. "An increase in the pleural thickness, however, suggests the likelihood of malignancy. A widening of the pleura of more than 1 cm is considered highly indicative of the presence of malignant tumor" (August 2004, Vol. 45:1 supplement, pp. S63-67).
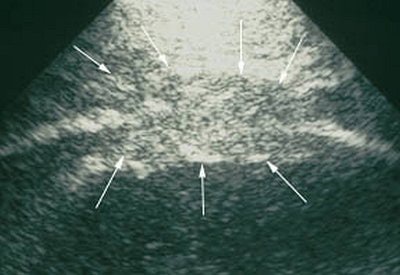 |
| Mesothelioma on ultrasound. Images courtesy of Dr. Felix Herth. |
Ultrasound can also aid in lung puncture technique, either as guidance for needle placement or for visualization of the entire procedure. Hertz recommended ultrasound over CT for these procedures as it enables continued monitoring, costs less, and does not pose a radiation risk.
Prognosis on FDG-PET
Unfortunately, the future can be very bleak for a patient assigned a clear-cut diagnosis of mesothelioma. The median survival rate for patients after diagnosis ranges from 12 to 18 months. Despite various possible treatment regimens, the mortality rate remains gloomy.
However, the type of mesothelioma that a person has can directly impact survival rates. Researchers from the University of Pennsylvania in Philadelphia demonstrated that FDG-PET had high sensitivity for assessing the extent of tumor involvement. Furthermore, they suggested tumor metabolic activity could correlate with survival.
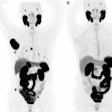
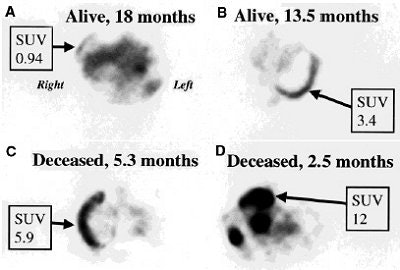 |
| Typical appearance of FDG PET studies in malignant mesothelioma. Transaxial slices were taken from four patients. Patient A, with tumor SUV of 0.94, was alive 18 months after PET scan. Patient B (SUV 3.4) was alive 13.5 months after PET. Patients C (SUV 5.9) and D (SUV 12) died shortly after PET scan, at 5.3 and 2.5 months, respectively. Reprinted by permission of the Society of Nuclear Medicine from Bernard F, Sherman D, et al, "Prognostic Value of FDG PET Imaging in Malignant Pleural Mesothelioma" (J Nucl Med 1999; 40: 1241-1245; p. 1244 [Figure 4]). |
In their study, 28 patients with suspected mesothelioma underwent FDG-PET scanning; the diagnosis was confirmed in 22 people. Standardized uptake values (SUVs) were determined from the most active tumor site in each patient.
According to the results, seven patients died during the follow-up period. The mean SUV of the deceased patients was 6.6 versus 3.2 among the combined survivors. The overall median SUV was 4.03, which was chosen as a cutoff to establish low-SUV and high-SUV groups. The survival distribution of the high-SUV group was shorter than the low-SUV group.
"This study clearly demonstrates that increased FDG uptake in mesothelioma is associated with an unfavorable prognosis," wrote Dr. Francois Benard and co-authors. "There is a trend toward lower FDG uptake in mesotheliomas of the epithelial subtype, generally thought to be a less aggressive form of disease" (Journal of Nuclear Medicine, August 1999, Vol. 40:8, pp.1241-1245).
One shortcoming of the study -- and others that have followed -- is a small patient population, noted Dr. Uwe Haberkorn from the University of Heidelberg in Germany. More research is needed to determine the best role for FDG-PET in mesothelioma, especially if it can be used to determine if invasive exploration is required.
"Possible applications of PET (include differentiating) between malignant and benign lesions in patients with asbestos exposure who present with atypical diffuse pleural thickening or pleural effusion," Haberkorn suggested. "PET may be helpful in deciding whether to pursue the investigation with thorascopy or thoracotomy" (Lung Cancer, August 2004, Vol. 45:1 supplement, pp. S73-76).
Pre- and post-treatment MRI
As with the two previous modalities, patients who are already contending with mesothelioma benefit most from MR imaging. Classifying asbestos-related pleural lesions with MR can be done, but is a tricky prospect as their appearance is similar in both benign and malignant disease, explained Dr. James Entwisle from Glenfield Hospital in Leicester, U.K.
Instead, he recommended deploying MR in two ways: as the final preoperative imaging exam before radical surgery and/or to assess postchemotherapeutic changes.
"Following radical surgery the hemithorax fills with fluid," he said. "The diaphragmatic patch is well-demonstrated on coronal MRI, and diaphragmatic defects are easily depicted" (Lung Cancer, August 2004, Vol. 45:1 supplement, pp. S69-71).
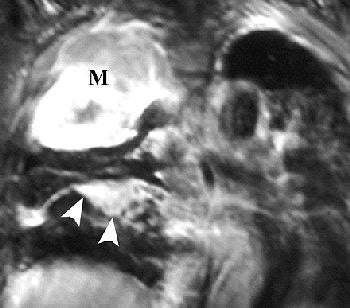
 |
R imaging evaluation of MPM in 63-year-old man. Coronal (top) and contrast-enhanced fat-saturated (below) T1-weighted MR images show a large, enhancing right apical mass with invasion of chest wall (black arrows, top). An enhancing right major fissure is also seen (white arrowheads, below). Figure 16, Wang ZJ, Reddy GP, et al, "Malignant Pleural Mesothelioma: Evaluation with CT, MR Imaging, and PET" (RadioGraphics 2004; 24: 105-119).
 |
Investigators from the University of California, San Francisco came to similar conclusions, advocating MR imaging in patients with potentially resectable disease.
"The excellent contrast resolution of MR imaging can allow improved detection of tumor extension.... Loss of fat planes, extension into mediastinal fat, and tumoral encasement of more than 50% ... are some of the features that suggest tumor extension," wrote Dr. Zhen Wang and colleagues in an educational exhibit for RadioGraphics (January-February 2004, Vol. 24:1, pp. 105-119).
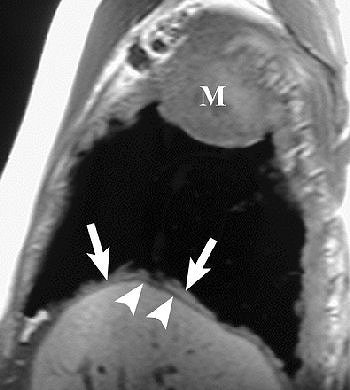 |
Sagittal T1-weighted (above) and coronal T2-weighted (below) MR images show the mass with involvement of the diaphragmatic pleura (arrows). However, there is no invasion of the diaphragmatic muscle itself (arrowheads). Figure 16, Wang ZJ, Reddy GP, et al, "Malignant Pleural Mesothelioma: Evaluation with CT, MR Imaging, and PET" (RadioGraphics 2004; 24: 105-119).
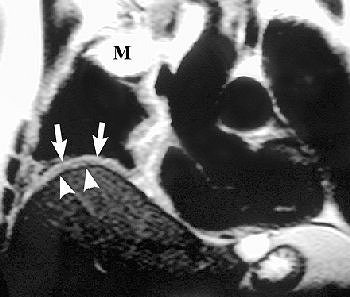 |
On T1-weighted MR images, malignant pleural mesothelioma (MPM) is typically isointense or hyperintense. On T2-weighted images, MPM is moderately hyperintense. In both cases, gadolinium enhances the disease, they added.
MRI may also prove superior for assessing the growth of MPM, either as an invasion of the diaphragm, invasion of the endothoracic fascia, or a single chest wall focus.
By Shalmali Pal
AuntMinnie.com staff writer
September 7, 2004
Related Reading
Part I: The back story on asbestos x-ray B readers, September 7, 2004
Court allows suit over radiologist's findings in pre-employment x-ray, August 20, 2004
Study sounds alarm over integrity of expert readers' testimony, August 6, 2004
ACR expels member for improper lawsuit testimony, July 9, 2004
Separating inflammation from malignancy on thoracic FDG-PET, April 9, 2004
Asbestos-related cancer on the rise in UK, February 2, 2004
Copyright © 2004 AuntMinnie.com