ORLANDO, FL - The post-therapy cancer protocol at many institutions is to watch and wait. If patients manifest elevated serum tumor markers such as S100 or carcinoembryonic antigen (CEA) during this follow-up period, conventional diagnostic methods call for the use of anatomic imaging first, then molecular imaging if necessary. A group in the Netherlands has flipped the imaging order, using PET as the primary imaging modality for occult tumors.
"We hypothesized that F-18 FDG-PET yields earlier recurrence detection, thus significantly altering clinical management," Dr. Judit Adam said.
Adam, a nuclear medicine physician from the department of nuclear medicine at the University of Amsterdam Academic Medical Center in the Netherlands, presented the results of a retrospective study conducted by researchers at her institution at the 2006 Academy of Molecular Imaging (AMI) scientific meeting on Monday morning.
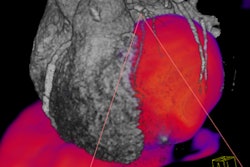
The group conducted FDG-PET scans on 44 patients (17 males and 27 females with a mean age of 58 years) who had a history of FDG-avid malignancy and elevated CEA or S100 tumor markers. All scans were conducted on an ECAT Accel lutetium oxyorthosilicate (LSO) crystal-based PET system (Siemens Medical Solutions, Malvern, PA), according to Adam.
The researchers retrospectively studied the clinical data, the FDG-PET outcome, and its influence on the clinical management of each patient for a median follow-up time of 11 months, Adam said. The team used conventional imaging after PET, pathological confirmation, and clinical follow-up as its gold standard, she said.
The researchers created two subgroups: one for the CEA marker representing gastrointestinal tumors (21 patients), and one for the S100 marker representing melanoma (15 patients).
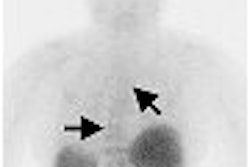
Overall, the team found 31 of the 44 patients to have FDG uptake that was suggestive for cancer recurrence. In 25 of these 31 patients, the uptake was true-positive, Adam said.
"In 60% of the cases, it led to an essentially altered clinical management, of which almost half was an intervention," she said.
In the S100 subgroup, 13 of the 15 patients were true-positive, and in 11 of the 13 cases, clinical management was altered on the basis of the FDG-PET results, Adam said. In the CEA subgroup, 13 of the 21 patients had true-positive results, and the PET outcome resulted in altered clinical management for 43% of these patients.
"Most of the PET-positive lesions were confirmed by conventional imaging; however, in some cases, there was a delay of up to two months to get these results," Adam noted.
In cancer patients in whom recurrence is suspected, such as when serum marker levels are elevated, the use of FDG-PET as a first-line imaging modality should strongly be considered, Adam believes, particularly if that cancer is melanoma.
"The most striking benefit was achieved in melanoma patients with elevated S100," she said. "Our data suggest that FDG-PET should be implemented up-front when occult tumor recurrence is suspected, especially in patients with melanoma."
By Jonathan S. Batchelor
AuntMinnie.com staff writer
March 29, 2006
Related Reading
PET/CT shows potential for detecting unknown primary cancers, December 8, 2005
Incidental focal findings on FDG PET/CT need follow-up endoscopy, September 6, 2005
PET/CT improves diagnostic accuracy of unexpected malignancies, June 30, 2005
Unexpected FDG-PET foci may signal subclinical tumors, December 26, 2002
FDG-PET signals early response of malignant GI tumors to Gleevec, July 1, 2002
Copyright © 2006 AuntMinnie.com