Historically, age and histology, as well as tumor volume and stage, have been used to predict patient outcome and overall survival for cervical cancer. But a multidisciplinary group from St. Louis-based Washington University School of Medicine has recommended the adoption of tumor uptake on FDG-PET imaging as a better biomarker for outcome and survival. They published the results of their study in Cancer.
"In cervical cancer, as in all cancers, overall survival is a key end point measure.... The results from recent studies in cancers of the head and neck, lung, and esophagus indicated that high FDG uptake in the primary tumor, typically characterized as a standard uptake value (SUV) greater than the median, predicts a worse outcome," wrote Dr. Elizabeth Kidd and colleagues. "In this study, we observed that the primary tumor SUVmax ... was a predictive biomarker of lymph node status, persistent disease after treatment, pelvic recurrence, and overall survival" (Cancer, September 4, 2007).
Kidd is from the university's department of radiation oncology. Her co-authors are Dr. Barry A. Siegel and Dr. Farrokh Dehdashti from the division of nuclear medicine, and Dr. Perry Grigsby from the division of gynecologic oncology.
For this investigation, 287 patients were included. Among the 287, 100 patients had Federation of Gynecology and Obstetrics (FIGO) stage IIB disease, with 89 patients having either stage IB1 or IB2 disease. According to pathology, there were 247 squamous cell carcinomas. At the time of diagnosis, 157 patients had involved lymph nodes. For treatment, 238 had a combination of external irradiation and intracavitary brachytherapy, as well as concurrent cisplatin chemotherapy.
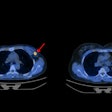
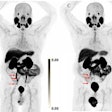
All patients underwent pretreatment FDG-PET or FDG-PET/CT scans for lymph node staging. The maximum pixel SUV within a region of interest encompassing the tumor was used, and the PET tumor volume of the cervical cancer was measured from the pretreatment image, the authors explained. The patients were imaged again at three months and the mean follow-up time was 32 months.
According to the results, the average SUVmax was 11.4 for all patients and 11.4 for patients treated with radiation. The average primary tumor SUVmax was 11.6 for squamous cell histology and 9.7 for nonsquamous histology.
The group found that SUVmax was the only significant independent predictor of death from cervical cancer. To analyze this association, patients were divided into three risk groups based on their primary tumor SUVmax. The authors calculated that patients with an SUVmax of 5.2 or less had an overall five-year survival rate of 95%. Patients with an SUVmax greater than 5.2 to 13.3 had a survival rate of 70%, and those with an SUVmax greater than 13.3 had a survival rate of 44%.
Of the 175 patients who underwent chemoradiation and three-month FDG-PET scanning, 19% had persistent disease and a higher primary cervical tumor SUVmax at diagnosis. "We observed that a higher primary tumor SUVmax significantly increased the risk of a pelvic recurrence and had some association with the development of distant disease," the group stated.
In addition, "the primary tumor SUVmax at the time of diagnosis was a more significant predictor of outcome in cervical cancer than FIGO stage, tumor volume, histology, or lymph node involvement."
Kidd's group said that, based on these results, the next step in their research will be prospective trials, targeting patients who present with elevated primary tumor SUVmax with more aggressive therapy.
By Shalmali Pal
AuntMinnie.com staff writer
September 19, 2007
Related Reading
Pilot study shows link between FDG uptake and biomarkers of cervical cancer, September 11, 2007
ROI can influence quantitative FDG-PET study results, September 11, 2007
Copyright © 2007 AuntMinnie.com