FDG-PET can replace conventional workup in primary M staging of nonkeratinizing nasopharyngeal carcinoma (NPC), according to researchers at Chang Gung University College of Medicine in Taipei, Taiwan.
NPC is etiologically linked with the Epstein-Barr virus and is endemic in southern China, Southeast Asia, the Middle East, North and East Africa, Greenland, and Alaska. The disease is characterized by early locoregional spread and a higher incidence of distant metastasis compared to other head and neck cancers.
Conventional workup (CWU) is done with chest radiography, abdominal ultrasonography, and skeletal scintigraphy to detect metastases, and although these techniques are available and affordable, they have limitations: Chest radiography does not detect mediastinal and hilar lymphadenopathies with the necessary sensitivity due to structure overlapping and inadequate soft-tissue contrast; ultrasonography is operator-dependent and distinguishing between benign and metastatic tumors can be difficult; and skeletal scintigraphy is not sensitive enough for detecting early bone or bone marrow metastasis.
Nonkeratinizing NPC responds to chemotherapy and radiation therapy, and finding early distant metastasis may improve survival outcomes with the application of proper treatment, according to the researchers. FDG-PET can image tumors with high glucose metabolisms, and has been shown to be useful for detecting distant metastasis and staging treatment, as well as detecting bone metastasis in NPC patients. But whether FDG-PET should be used as an adjunct to conventional workup or can replace it has not been clear.
In a study published in the Journal of Nuclear Medicine, Dr. Tzu-Chen Yen, Ph.D., and colleagues compared the diagnostic efficacies of FDG-PET and conventional workup, as well as a combination of the two (JNM, October 2007, Vol. 48:10; pp: 1614-1619).
The study included 300 patients diagnosed with histologically proven nonkeratinizing NPC between April 2002 and August 2005, and with no prior treatment. All underwent conventional workup and FDG-PET for primary M staging within two weeks after joining the study. Mean age was 50 years, and the male-to-female ratio was 2-to-1.
Chest radiography was done according to standard protocol and interpreted by the attending radiologist. Abdominal sonography was performed and interpreted by the attending physician, with the liver as the primary target. Skeletal scintigraphy was performed with a dual-head gamma camera with general-purpose collimators. All the participants in the study fasted for at least six hours before the FDG-PET exam.
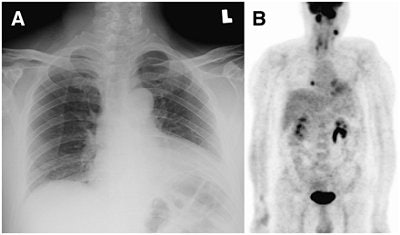 |
| A 49-year-old man who was a patient with NPC of stage T4 N2. (A) Chest radiography revealed no evidence of chest metastasis. (B) Maximum intensity projection image of F-18 FDG-PET revealed focal metastasis in right lower chest. CT-guided biopsy of 0.8-cm nodule in right lower lung confirmed it to be a metastatic tumor. "18-F-FDG PET Can Replace Conventional Work-up in Primary M Staging of Nonkeratinizing Nasopharyngeal Carcinoma" (Journal of Nuclear Medicine, Vol. 48:10, pp. 1614-1619). Reprinted by permission of SNM. |
Distant metastasis was considered to be present if one or more of the following conditions were met within one year of the primary diagnosis: histologic proof of distant metastases, unequivocal evidence of distant metastases in the imaging studies, and equivocal evidence of distant metastases in the imaging studies that was subsequently proved histologically or via clinical progression. The metastasis sites were grouped into four regions: the skeleton, thorax, liver, and other sites.
Of the 300 patients, 61% had distant metastases: 48 (16%) had skeletal metastases, 27 (9%) had chest metastases, 23 (7.7%) had hepatic metastases, 15 (5%) had metastases involving other sites, and 29 patients had metastases in two or more regions.
The group found that FDG-PET had an impact on the management of 39 patients: 31 were upstaged and eight were downstaged. Seven patients were falsely upstaged and one patient was falsely downstaged by FDG-PET.
On a patient-based analysis, Yen and colleagues found that FDG-PET was more effective than conventional workup, but was equally effective when used in combination with conventional workup. Among those study participants with distant metastases, 50 (82%) were detected by FDG-PET and 20 (32.8%) were detected by CWU. PET combined with conventional workup was slightly more sensitive (83.6%), but with a cost to specificity and accuracy.
|
||||||||||||||||||||
In a region-based analysis, FDG-PET was better than skeletal scintigraphy and chest radiography for detecting bone and chest metastases. FDG-PET and abdominal ultrasound were equally effective for detecting hepatic metastases, but PET combined with contentional workup did not yield higher area-under-curve (AUC) values in both patient- and region-based analyses.
FDG-PET is superior to conventional workup in primary M staging of nonkeratinizing NPC patients, and can replace conventional workup, the authors concluded.
By Kate Madden Yee
AuntMinnie.com staff writer
November 15, 2007
Related Reading
FDG-PET, MRI show worth in tumor treatment response, November 2, 2007
SUV on FDG-PET can predict cervical cancer prognosis, September 19, 2007
Pilot study shows link between FDG uptake and biomarkers of cervical cancer, September 11, 2007
ROI can influence quantitative FDG-PET study results, September 11, 2007
Fused MRI and PET improve specificity of breast MRI, August 17, 2007
Copyright © 2007 AuntMinnie.com