Much has been researched and written about the promise of PET/MRI. While the hybrid modality's range of clinical applications appears expansive, the authors of an editorial published online February 7 in the Journal of Nuclear Cardiology pose the opinion that it might be time to pump the brakes on wider use of PET/MRI, at least in cases of cardiac sarcoidosis.
In the piece, Dr. Zorana Mrsic, from Walter Reed National Military Center in Bethesda, MD, and Dr. Edward Hulten, from Fort Belvoir Community Hospital in Fort Belvoir, VA, weigh the pros and cons of PET/MRI, balancing its clinical efficacy with operational realities.
"Although the hybrid PET/MRI technique has sparked tremendous interest and enthusiasm, it is important to pause and ask certain questions regarding the benefits, disadvantages, applicability, accessibility, and cost-effectiveness of this technology," they wrote.
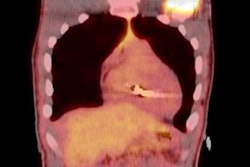
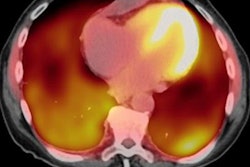
Cardiac sarcoidosis is an inflammatory disease that can adversely affect heart function and lead to morbidity and mortality. Previous studies have shown the modalities together and separately offer distinct and complementary patient data. FDG-PET can detect myocardial inflammation and compensate for cardiac MRI's lack of diagnostic accuracy. At the same time, cardiac MRI can better characterize tissue in areas of increased edema, fibrosis, or scarring through pre- and postgadolinium-based contrast.
A handful of studies with small patient cohorts have evaluated PET/MRI in this regard. A December 2015 study by Hanneman et al found that when paired with MRI, PET achieved positive results for cardiac sarcoidosis for all eight patients (100%), compared with only four patients (50%) with PET/CT.
More recently, a January 2019 study of 10 patients by Wisenberg et al concluded that PET/MRI provided diagnostic-quality FDG images that were "at least equal to or better than those obtained with either the PET/CT scan, and subjectively crisper MR images" than those from a 1.5-tesla MRI scanner (J Nucl Cardiol, January 2, 2019).
These studies, while "eloquently designed," touch just the tip of the iceberg when determining the appropriateness of PET/MRI use, Mrsic and Hulten cautioned. On one hand, PET/MRI reduces the amount of ionizing radiation exposure to patients by eliminating a CT scan. Notable beneficiaries would include young patients with cardiac sarcoidosis who face a series of imaging scans.
On the other hand, many cardiac sarcoidosis patients have implantable cardiac devices (ICDs). It is unlikely that will change, given that, for one, the Heart Rhythm Society recommends defibrillator implantation as a preventive remedy for patients with the condition due to their high incidence of ventricular arrhythmia and sudden cardiac death.
Although MRI-conditional pacemakers and ICDs may be safely scanned, they still require pre- and postscan interrogation for MR imaging and additional precautions, and they contain metal that results in more significant image artifacts on PET/ MRI versus PET/CT, the authors wrote.
In addition, economic considerations and "operational obstacles" can impede utilization of the technology. The obstacles include the greater costs of purchasing and operating the hybrid scanners and a lack of technologists trained in both modalities, which has stunted PET/MRI's adoption, Mrsic and Hulten asserted.
"The true generalizability of hybrid PET/MRI for cardiac sarcoidosis, therefore, remains in question," they added. "Although the potential benefits are undeniable, the practical value in patients with suspected or confirmed cardiac sarcoidosis is yet to be determined."