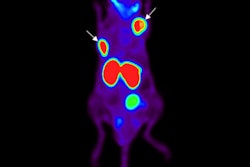
When a prostate cancer staging exam is needed, clinicians at one Australian hospital are overwhelmingly choosing PET/CT with the radiopharmaceutical gallium-68 (Ga-68) prostate-specific membrane antigen (PSMA), according to a study published online April 11 in the Journal of Medical Imaging and Radiation Oncology.
Six months after The Wesley Hospital in Brisbane, Queensland, began performing Ga-68 PSMA PET/CT scans, the average number of monthly bone scintigraphy studies plummeted by almost 50% in favor of Ga-68 PSMA PET/CT. Five years later, clinicians turned to Ga-68 PSMA PET/CT for the primary and secondary staging of prostate cancer in 95% of their cases.
"As far as we are aware, this study is the first to show the declining use of nuclear medicine bone scans with the introduction of PSMA-PET/CT in the urological community," wrote the researchers, led by Crishan Haran, from the University of Queensland. "This is significant not only because PSMA-PET/CT examinations represent a new paradigm in prostate cancer staging but also because Australia is one of the world leaders in the use of PET imaging."
Imaging options
For many years, whole-body bone scintigraphy with technetium-99m (Tc-99m) methylene diphosphonate was the standard modality for determining the presence of bone metastases in prostate cancer. More recently, clinicians explored PET with FDG or choline for prostate cancer staging, but these approaches had limitations due to tracer uptake into normal or benign tissue or cells. Hence, ligands, which target the prostate-specific membrane antigen, were developed because PSMA is considerably more abundant in cancerous prostate cells than in normal prostate cells. PSMA is also proportionally expressed in relation to the grade and stage of prostate cancer, making it an "attractive target" for radiotracers, the researchers added.
In their study, Haran and colleagues wanted to fill a research gap.
"Despite the ongoing evaluation of the performance of PSMA-PET/CT, in particular, compared [with] nuclear medicine bone scans and CT imaging, there is little information regarding the use of these modalities in the real world by clinicians," they wrote. "Therefore, in this study, we aim to describe the trends of use between PSMA-PET/CT and nuclear medicine bone scans by urologists for both primary and secondary staging of prostate cancer in the first institution in Australia to offer both modalities."
Modality popularity
The researchers reviewed prostate cancer staging and restaging cases by modality at their private tertiary hospital between January 2013 and April 2018. PSMA-PET/CT scans were performed using a Ga-68 PSMA radiotracer, while bone scintigraphy scans were conducted with SPECT and Tc-99m methylene diphosphonate (J Med Imaging Radiat Oncol, April 11, 2019).
Over the study's five years, clinicians performed 3,144 exams for staging and/or restaging of prostate cancer, including 2,598 PSMA-PET/CT scans (83%) and 546 scintigraphy bone scans (17%). The exams were performed on a total of 2,693 patients, with 453 individuals (17%) having more than one scan and 260 people (9%) undergoing both scintigraphy and PSMA-PET/CT.
As the researchers charted the frequency of scans per modality on a monthly basis, they observed a significant decline in the average number of bone scintigraphy exams from the start of the study in July 2014 (21.5 exams) to an average of only one exam in the final six months of the study.
| Average No. of scans per month by modality | |||
| Bone scintigraphy | Decrease* | PSMA-PET/CT | |
| Before PSMA-PET/CT | 21.5 | ||
| 6 months later | 12 | 45.7% | 61 |
| Final 6 months of study period | 1 | 95.3% | 53 |
PSMA-PET/CT reached its peak with 74 scans in November 2014, four months after its launch. Of all 2,598 PSMA-PET/CT exams, 1,569 scans (60%) were conducted for primary staging, compared with 1,029 exams (40%) for secondary staging.
A further breakdown found that the first 500 PSMA-PET/CT exams included 246 scans (49%) performed for primary staging. As clinicians presumably felt more comfortable administering the exams over time, the number of exams increased to 347 (69%) for primary staging, based on the final 500 PSMA-PET/CT scans in the study period, according to the researchers. That gain was a statistically significant increase (p < 0.05).
Trailblazing experience
The attraction of The Wesley Hospital clinicians to PSMA-PET/CT could be viewed as somewhat unusual. As they noted in their paper, when the facility began using the modality in July 2014, the U.K.'s National Institute for Health and Care Excellence, the American Urological Association, and the European Association of Urology (EAU) did not mention the use of PSMA-PET/CT for staging prostate cancer.
"Instead, all [of the organizations] suggested the use of either multiparametric MRI, abdominopelvic CT, and/or nuclear medicine bone scans depending on the patient's risk factors," Haran and colleagues wrote. "Indeed, on reviewing the most recent iterations of these guidelines, only the EAU makes note of the evolving role of PSMA-PET/CT for initial staging but continues to recommend the use of nuclear medicine bone scans and abdominopelvic CT."
So what makes these Australian clinicians different? Even they aren't sure why.
"One possible reason is due to the heavy research focus within both our nuclear medicine and urological departments and a willingness of clinicians to trial new imaging modalities," they conjectured.
Previous research also found that fluctuating prostate-specific antigen (PSA) levels can cause a delay in the detection and diagnosis of metastatic prostate cancer with bone scintigraphy and CT. In addition, nuclear medicine bone scans are known to have limited sensitivity at low PSA levels, which leaves a "grey area for clinicians who observed a low (< 10 ng/mL) but rising PSA in patients with previously treated prostate cancer," Haran and colleagues wrote.
"This grey area was able to be filled with PSMA-PET/CT and likely reflects why in the initial cohort of 500 patients [in the current study], PSMA-PET/CT was used for secondary staging at a similar rate to primary staging," the authors added. "As confidence in PSMA-PET/CT rose, its use for pretreatment staging increased, reflected in the significant difference in use for primary staging seen when comparing the first and final 500 patients."
Given these results, Haran and colleagues believe their transformative experience with the modality will be replicated at other institutions.