PET/MRI scans show middle-aged adults with high vascular risk factors have less whole-brain volume by the time they reach their late 60s, but their lifestyle and physical characteristics do not influence beta-amyloid accumulation, according to a study published online November 4 in JAMA Neurology.
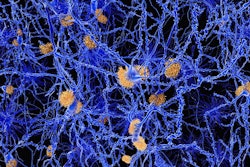
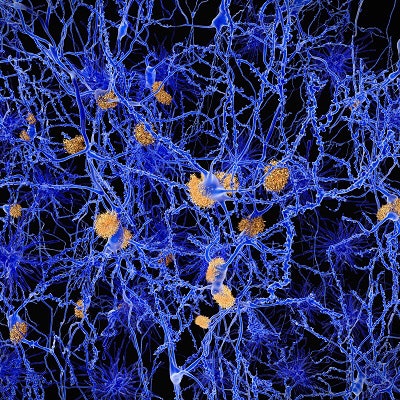
The results confirm the need for a concerted reduction in vascular risk factors in middle age, such as hypertension, smoking, diabetes, and obesity, to help ensure a healthier brain later in life. Perhaps more importantly, the researchers found no connection between these risk factors among subjects in their 30s and beta-amyloid accumulation over the next several decades, which is associated with a progression to cognitive decline dementia.
"[The] findings support that while midlife is an important period of risk exposure, influences of vascular risk on brain structure extend back into early adulthood and may be particularly damaging at this time or may alternatively reflect increased accumulated risk exposure," wrote lead author Dr. Christopher Lane, PhD, and colleagues from University College London and King's College London in the U.K.
For this study, the researchers took data from participants in the U.K. Medical Research Council National Survey of Health and Development (NSHD) who had their vascular risk factors quantified through Framingham Heart Study (FHS) cardiovascular risk scores (CVS), which measure the risk of a cardiac event at ages 36, 53, and 69. Along with those assessments, subjects' socioeconomic status, apolipoprotein E (APOE) ε4 genotype, and whole-brain and hippocampal volumes were recorded.
They also underwent simultaneous PET/MRI scans (Biograph mMR, Siemens Healthineers) between ages 69 and 71 from May 2015 to January 2018. The 3-tesla MRI protocol included volumetric T1-weighted and fluid-attenuated inversion-recovery (FLAIR) sequences, while beta-amyloid burden was assessed using PET imaging with the radiopharmaceutical florbetapir (Amyvid, Avid Radiopharmaceuticals), which is designed to adhere to and identify beta-amyloid plaques.
"This [NHSD data] allowed us to investigate the influence of vascular risk exposure timing on brain structure and pathology at age 69 to 71 years, with a specific focus on cerebral small-vessel disease, beta-amyloid deposition, and brain volumes, using measures from early adulthood, midlife, and early late life," Lane and colleagues wrote.
Their analysis included 463 people (mean age, 70.7 ± 0.7 years) with no signs of dementia and who had completed all the aforementioned protocols. Of those subjects, 455 individuals (90.6%) were available for amyloid analysis, 83 (18.2%) of whom were beta-amyloid positive (and met the inclusion criteria); 443 subjects (88.2%) for brain-volume analysis; and 451 participants (89.8%) for volume analysis of white-matter hyperintensities.
Cardiovascular connection
Through the analyses, Lang and colleagues discovered that FHS-CVS scores, which rated the 10-year risk of a cardiac event, increased at each subsequent age point, while MR images revealed decreases in whole-brain volumes and greater white-matter hyperintensity volume -- a proxy marker of cerebral small-vessel disease. At the same time, they found no associations between vascular risk scores at any time point and a subject's beta-amyloid status on PET scans.
| Effects of vascular risk factors relative to vascular risk scores | |||
| 36 years | 53 years | 69 years | |
| Framingham 10-year risk of cardiac event | 2.7% | 10.9% | 24.3% |
| Whole-brain volume* | -3.6% | -0.8% | -0.6% |
| Mean hippocampal volume* | -0.03 | -0.0001 | -0.0001 |
| White matter-hyperintensity volume** | 1.09 | 1.02 | 1.01 |
| Beta-amyloid status*** | 0.98 | 0.97 | 0.99 |
**Measured by exponentiated coefficient
***Adjusted odds ratio
The researchers interpreted the data to mean that vascular risk at ages 69 to 71 as demonstrated by white-matter hyperintensity volume and brain volume increases the earlier that vascular risk is present -- with the strongest risk being at age 36.
In an accompanying editorial published in JAMA Neurology, Dr. Sudha Seshadri, from the Glenn Biggs Institute for Alzheimer's and Neurodegenerative Diseases at the University of Texas Health San Antonio, emphasized "three less expected and, hence, intriguing observations" from the study.
Seshadri cited that early adulthood vascular risk exposure was greater in women, which led to a greater risk of later-life dementia among female subjects. At the same time, women had lower 10- and 20-year risks of cardiovascular events compared with men, "but conversely, they may be more vulnerable than men to subtle brain injuries that increase dementia risk several decades later," she wrote.
The level of vascular risk factors in late life appeared to be less harmful and could be associated with fewer MRI-detected abnormalities.
The researchers found no association of vascular risk in early or middle adult life with brain amyloid plaque depositions at age 70, which "remains a controversial area for which further study is urgently required," Seshadri concluded.