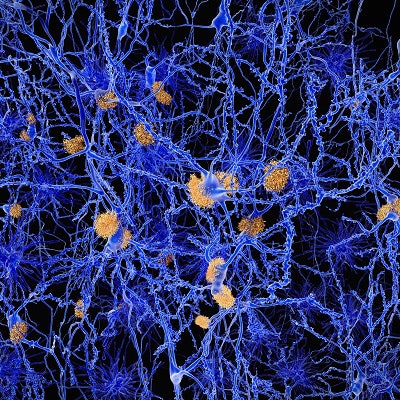
Initial findings from the Anti-Amyloid Treatment in Asymptomatic Alzheimer's Disease (A4) study, published online April 6 in JAMA Neurology, have confirmed that high levels of amyloid on florbetapir-PET brain scans are an indication of cognitive decline.
A4 study researchers analyzed some 4,500 clinically normal older adults with elevated amyloid deposits on PET scans. Researchers found worsening cognitive capabilities and diminishing daily function that could signal the onset of Alzheimer's disease.
"These results support the hypothesis that elevated amyloid represents an early stage in the Alzheimer continuum and demonstrate the feasibility of enrolling these high-risk participants in secondary prevention trials aimed at slowing cognitive decline during the preclinical stages of Alzheimer's disease," wrote the authors, led by Dr. Reisa Sperling from the Center for Alzheimer Research and Treatment at Brigham and Women's Hospital in Boston.
There are 67 clinical trial sites in the U.S., Canada, Australia, and Japan contributing data to the 240-week Anti-Amyloid Treatment in Asymptomatic Alzheimer study. The researchers began in 2014 to screen for eligible participants who are between 65 and 85 years of age, cognitively normal, living on their own, and have a study partner who also provides information on the subject's daily cognitive function throughout the year.
Among the goals of the A4 study is to determine whether Eli Lilly's investigational drug solanezumab can slow cognitive decline in people with amyloid accumulation if the regimen begins before clinical symptoms appear. The researchers hope to complete the A4 study in late 2022.
"This first report of the A4 study screening experience focuses on amyloid eligibility, a comparison of the [beta-amyloid positive] and [beta-amyloid negative] cognitively normal groups on demographic and lifestyle factors, and the primary cognitive and functional outcome measures obtained during screening," Sperling and colleagues wrote.
This portion of the A4 study included 4,486 eligible participants (mean age, 71.3 ± 4.7 years) who underwent amyloid-PET imaging with florbetapir (Amyvid, Avid Radiopharmaceuticals). Standardized uptake value ratios (SUVr) between 1.10 and 1.15 were considered indicative of elevated amyloid levels. The researchers also compared, among other key characteristics, the subjects' demographic data, family history, and the presence of the dementia-contributing apolipoprotein E (APOE) ε4 genotype.
In addition, a 15-question survey, known as the Cognitive Function Index (CFI), was given to each person and their study partner to gauge the participant's daily capabilities. The CFI is based on a scale of 0 to 18, with higher scores indicating worse cognition.
Florbetapir-PET revealed 1,323 people (29%) who were positive for beta-amyloid accumulation, compared with 3,163 beta-amyloid-negative subjects (70%). The beta-amyloid-positive participants also were significantly older, had a history of family dementia, and showed at least one APOE ε4 genotype.
The beta-amyloid-positive group also reported significantly greater subjective declines in cognitive function over the year on the CFI questionnaire, with APOE ε4 carriers noting higher CFI scores than noncarriers in both beta-amyloid groups.
| Significant differences between beta-amyloid positive and negative subjects | |||
| Beta-amyloid-positive subjects | Beta-amyloid- negative subjects | p value* | |
| No. of subjects | 1,323 (29%) | 3,163 (71%) | < 0.001 |
| Mean age | 72.1 years | 70.9 years | < 0.001 |
| Family history of dementia | 976 (74%) | 2,137 (68%) | 0.001 |
| At least 1 APOE ε4 | 105 (8%) | 34 (1%) | < 0.001 |
| SUVr | 1.33 | 0.99 | < 0.001 |
| Self-reported CFI | 2.20 | 2.01 | < 0.001 |
SUVr: standardized uptake value ratio
Interestingly, the researchers noted that even with the significant associations between poor cognitive performance and these contributing factors, it "remains challenging to use any one of these variables to accurately predict amyloid status given the relatively modest effect size. Work is ongoing to determine whether some combination of test scores, subjective reports, family history, genetic testing, and eventually blood-based biomarkers of amyloid and tau can improve the accuracy of predicting amyloid status in cognitively unimpaired individuals, perhaps particularly among APOE noncarriers."