PET and MR images have revealed four significant differences in the brains of middle-aged women and men that may shed light on why females are more susceptible to Alzheimer's disease, according to a study published online June 24 in Neurology.
The disparities included the presence of more Alzheimer's-associated beta-amyloid plaque in the brains of women compared with men. The women also exhibited significantly lower glucose metabolism as measured by FDG uptake, with gender and menopausal status the two most consistent predictors of FDG uptake. Women also had less gray and white brain matter volume than men (Neurology, July, 24, 2020; Vol. 95:2, pp. 1-13).
"Our findings suggest that middle-aged women may be more at risk for the disease, perhaps because of lower levels of the hormone estrogen during and after menopause," said study co-author Lisa Mosconi, PhD, of Weill Cornell Medicine, in a statement. "While all sex hormones are likely involved, our findings suggest that declines in estrogen are involved in the Alzheimer's biomarker abnormalities in women we observed. The pattern of gray matter loss in particular shows anatomical overlap with the brain estrogen network."
Mosconi and colleagues have been active for several years in researching the development of Alzheimer's disease in women. Their 2017 study used PET to discover a possible relationship between menopausal status and metabolic indications of Alzheimer's. Their three-year longitudinal study, published in 2018, investigated whether a woman's age, menopausal status, and levels of beta-amyloid plaque on PET scans could be combined as biomarkers to determine the best time to begin treatment to slow the onset of Alzheimer's disease.
There have been, however, "no studies [that] have examined how sex-specific risks affect Alzheimer's-related brain changes in midlife and which are most impactful," the authors wrote. "Brain biomarkers are crucial to this aim, because there is extensive evidence that they can detect presence of Alzheimer's decades before clinical symptoms."
For this study, the researchers analyzed 85 women (53 ± 6 years) and 36 men (52 ± 8 years) with no cognitive impairment, as well as similar characteristics such as vascular risk factors, thyroid function, family history, physical lifestyles, and memory skills.
All participants underwent PET imaging with carbon-11-labeled Pittsburgh Compound B (PiB) to detect beta-amyloid protein, which is associated with the onset of Alzheimer's; FDG to determine the degree of neurodegeneration; and structural MRI to measure the brain's white and gray matter.
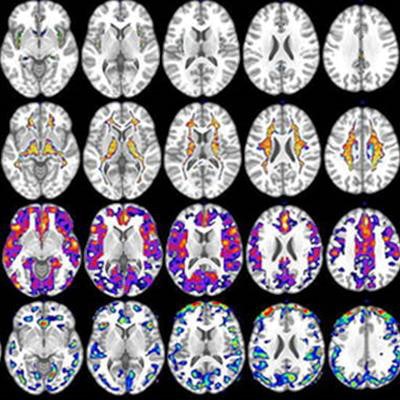
PET and MRI, respectively, revealed statistically significant differences (p < 0.05) between the genders in four categories. The women presented with the following:
- 30% more beta-amyloid plaques in women on average in the brain than men
- 22% less glucose metabolism, primarily in the superior frontal gyrus, medial frontal gyrus, and inferior parietal lobule
- 11% less gray matter volume (0.73 cm3) on average in women, compared with men (0.8 cm3)
- 11% less white matter volume (0.74 cm3) on average in women than men (0.82 cm3)
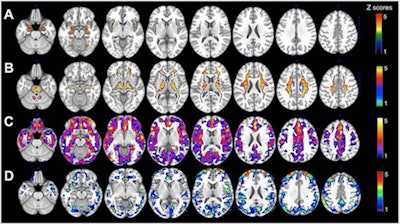 (A) MRI gray-matter volumes. (B) MRI white-matter volumes. (C) Pittsburgh compound B-PET beta-amyloid deposition. (D) FDG-PET glucose metabolism. Statistical parametric maps (SPMs) displaying brain regions showing Alzheimer's disease biomarker abnormalities in women versus men are represented on different color-coded scales after being thresholded to standardized z scores: 1 < z < 5, where z > 3 corresponds to p < 0.05 family-wise error corrected. All SPMs are displayed onto a standardized MR image. Image courtesy of Neurology, the medical journal of the American Academy of Neurology.
(A) MRI gray-matter volumes. (B) MRI white-matter volumes. (C) Pittsburgh compound B-PET beta-amyloid deposition. (D) FDG-PET glucose metabolism. Statistical parametric maps (SPMs) displaying brain regions showing Alzheimer's disease biomarker abnormalities in women versus men are represented on different color-coded scales after being thresholded to standardized z scores: 1 < z < 5, where z > 3 corresponds to p < 0.05 family-wise error corrected. All SPMs are displayed onto a standardized MR image. Image courtesy of Neurology, the medical journal of the American Academy of Neurology.Interestingly, despite the aforementioned differences, the researchers found no reduction in cognitive performance in women compared with men, including postmenopausal and perimenopausal women. The researchers suggested this finding supported the "notion that brain biomarkers are more sensitive than cognitive tests for the detection of Alzheimer's risk in asymptomatic individuals."
Mosconi and colleagues conclude that the results are "pertinent to healthy, middle-aged participants without severe cerebrovascular or cardiovascular disease. Studies with larger samples, longitudinal follow-ups, and community-based populations are necessary to assess the generalizability of these findings."