Researchers from the H. Lee Moffitt Cancer Center and Research Institute in Tampa, FL, have reported that CT radiomics features can help predict tumor behavior in screening-detected lung cancer. They've also found that PET/CT radiomics shows promise for guiding non-small cell lung cancer (NSCLC) treatment decisions.
In a presentation at the recent virtual 2020 North American Conference on Lung Cancer, Moffitt researchers led by first author Jaileene Pérez-Morales, PhD, reported that the combination of two CT radiomics features and a tumor volume doubling time (VDT) threshold yielded a high degree of accuracy for predicting survival outcomes.
"Utilizing VDT and radiomic features, decision tree analysis identified subsets of screen-detected lung cancers associated with very poor survival outcomes suggesting such patients may [need] more aggressive treatment, such as adjuvant therapies, and more aggressive surveillance/follow-up," the authors wrote.
Predicting cancer outcomes
The researchers sought to make use of radiomics features and tumor volume doubling time to generate parsimonious models for predicting lung cancer outcomes in cases identified from lung cancer screening. Using patient data and low-dose CT images from incidentally detected lung cancer patients from the National Lung Screening Trial (NLST), they first calculated VDT as the difference between two LDCT exams performed approximately one year apart.
Next, they extracted 155 intratumoral and 109 peritumoral radiomic features from the LDCT exams. After performing classification and regression tree (CART) analyses using overall survival as the main endpoint, the researchers found that the best predictive performance was achieved by using a combination of a tumor VDT threshold of 234 days and two CT radiomics features -- compactness and average co-occurrence.
With this combination, decision-tree analysis was then employed to stratify patients into low-, intermediate-, high-, and very-high-risk categories. The researchers found significant differences in outcomes between early-stage patients classified by the multivariable model into low- and very-high risk categories.
| Outcomes measures in screening-detected lung cancer patients by model risk category | ||||
| Low-risk patients overall | Very-high-risk patients overall | Low-risk early-stage patients | High-risk early-stage patients | |
| Hazard ratio | 1.00 | 11.96 | 1.00 | 15.2 |
| 5-year overall survival | 82.4% | 21.4% | 90.6% | 33.3% |
After 10-fold cross-validation was performed, this model yielded an area under the curve (AUC) of 0.84 for predicting patient outcomes.
PET/CT radiomics in NSCLC
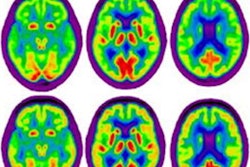
Senior author Matthew Schabath, PhD, also served in that role in another recent Moffitt study that detailed how a deep-learning algorithm could utilize PET/CT radiomics to identify the best treatment option for NSCLC patients. The researchers shared their findings in an article published online October 16 in Nature Communications.
In that project, the group retrospectively used F-18 FDG PET/CT data from two hospitals in China for training a deep-learning model to classify a NSCLC patient's epidermal growth factor (EGFR) mutation status, an important predictor for treatment. Patients with an active EGFR mutation status respond better to tyrosine kinase inhibitor (TKI) treatment than immune checkpoint inhibitor (ICI) therapy.
After analyzing the images, the model generates a EGFR deep-learning score to classify their EGFR mutation status. The researchers subsequently tested the algorithm on patient data from a different hospital in China as well as Moffitt.
The deep-learning score yielded an AUC of 0.81 on the training set for discriminating between EGFR-mutant type from wild type, significantly higher than the AUC of 0.50 produced by the commonly used SUVmax measure, according to the authors.
Progression-free survival
What's more, progression-free survival was significantly longer (p = 0.01) in TKI-treated patients who had a high EGFR deep-learning score than those who had a low deep-learning score. Conversely, patients who had lower deep-learning scores and who had received immune checkpoint inhibitor treatments also had significantly longer progression-free survival than those with higher deep-learning scores (p < 0.001).
"We found that the EGFR deep-learning score was positively associated with longer progression-free survival in patients treated with tyrosine kinase inhibitors, and negatively associated with durable clinical benefit and longer progression-free survival in patients being treated with immune checkpoint inhibitor immunotherapy," said co-author Robert Gillies, PhD, in a statement. "We would like to perform further studies but believe this model could serve as a clinical decision support tool for different treatments."
Prior studies have utilized radiomics as a noninvasive approach to predict EGFR mutation status, noted first author Wei Mu, PhD.
"However, compared to other studies, our analysis yielded among the highest accuracy to predict EGFR and had many advantages, including training, validating and testing the deep learning score with multiple cohorts from four institutions, which increased its generalizability," she said in a statement.