An artificial intelligence (AI) algorithm that significantly reduces PET imaging time and radiation dose in cancer patients is as effective as standard PET exams -- and the method produces similar results regardless of the scanner model, according to a study in npj Digital Medicine.
If applied clinically, the AI algorithm could reduce radiation dose for patients and lower the cost of PET imaging, the authors suggest.
"The proposed low-count-enhancement technique is promising to enable lower radiotracer dose and to improve the efficiency of diagnostic PET imaging," wrote first author Dr. Akshay Chaudhari of Stanford University in Menlo Park, CA, and colleagues.
PET imaging is limited by its high cost and radiation dose, but reducing PET scan time or radiotracer dosage usually degrades diagnostic image quality, according to the authors. Preliminary studies have assessed AI methods for enhancing image quality, yet none have been tested in a realistic clinical setting, and the impact on quantitative standardized uptake value (SUV) measurements has not been robustly validated across vendors and reconstruction algorithms, the authors stated.
In this prospective study, a team of researchers evaluated the performance of an AI algorithm (SubtlePET, Subtle Medical) when applied to fourfold reduced-count whole-body PET in a realistic clinical environment with multiple blinded readers, institutions, and scanner types.
The researchers enrolled 26 men and 24 women from three separate hospitals who were referred for standard whole-body FDG PET/CT exams for cancer diagnoses between September 2018 and April 2019. Low-count scans were either captured from a separate scan with fourfold shorter bed durations performed immediately following the standard scan or were created by reconstructing shorter bed durations from the standard scan using list-mode data.
Three board-certified nuclear medicine physicians with seven, 12, and 22 years of experience at three separate academic institutions evaluated the efficacy of the low-count-enhanced PET scans. The readers evaluated two sets of PET scans per patient. One set consisted of the original 100% full-count PET scans ("standard") and one set consisted of 25% low-count PET scans enhanced using the AI software.
The readers detected a combined total of 491 hypermetabolic lesions in 92 total standard scans. The number of hypermetabolic lesions identified on the standard and low-count enhanced scans was not statistically different, the authors found.
The overall patient-level sensitivity and specificity for detecting lesions on the low-count-enhanced scan compared with the standard scan were 0.94 and 0.98. Interscan kappa agreement of 0.85 was comparable to intrareader (0.88) and pairwise interreader agreements (maximum of 0.72). SUV quantification was comparable in the reference regions and lesions and had high correlation.
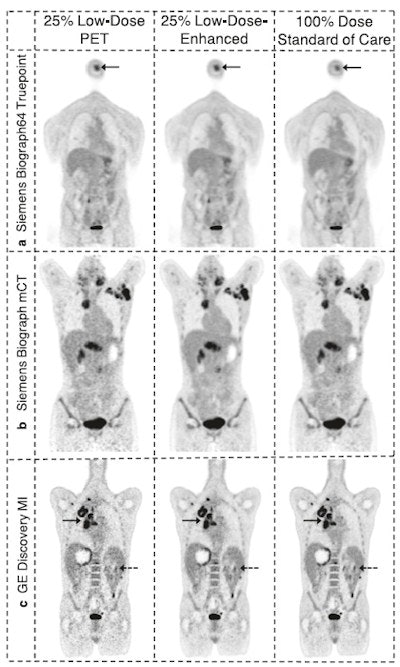 Example 25% low-count PET images, the 25% low-count-enhanced images, and the corresponding standard images for all three scanners for subjects with body mass index (BMI) under 30. (A) A 66-year-old male with BMI of 27 scanned on a Siemens Biograph 64 TruePoint for oropharyngeal cancer (solid arrow pointing to a distant lung metastasis). (B) A 34-year-old female with BMI of 20 scanned on a Siemens Biograph mCT for lymphoma (solid arrow pointing to metastatic lymph nodes and dashed arrow pointing to lesion in the spleen). (C) A 58-year-old male with BMI of 23 scanned on a GE Discovery MI with lung cancer (solid arrow). For all subjects, all low-count images appear considerably noisier compared with the low-count-enhanced and standard images. Note: SUV display scale is 0-7. Image courtesy of npj Digital Medicine.
Example 25% low-count PET images, the 25% low-count-enhanced images, and the corresponding standard images for all three scanners for subjects with body mass index (BMI) under 30. (A) A 66-year-old male with BMI of 27 scanned on a Siemens Biograph 64 TruePoint for oropharyngeal cancer (solid arrow pointing to a distant lung metastasis). (B) A 34-year-old female with BMI of 20 scanned on a Siemens Biograph mCT for lymphoma (solid arrow pointing to metastatic lymph nodes and dashed arrow pointing to lesion in the spleen). (C) A 58-year-old male with BMI of 23 scanned on a GE Discovery MI with lung cancer (solid arrow). For all subjects, all low-count images appear considerably noisier compared with the low-count-enhanced and standard images. Note: SUV display scale is 0-7. Image courtesy of npj Digital Medicine."All three readers who analyzed the diagnostic utility of the two sets of PET scans consistently rated the low-count enhanced scans as noninferior to the standard scans," the researchers wrote.
The findings in this study are more clinically relevant compared to previous low-count PET-enhancement methods since the cohort consisted of patients with varying pathologies who were assessed by board-certified nuclear medicine physicians, the authors added.
"Overall, this method may enable either dose or exam-duration reduction, increasing safety and lowering the cost of PET imaging," they concluded.