PET imaging with a radiotracer based on prostate-specific membrane antigen (PSMA) can help predict whether patients with metastatic prostate cancer will respond to chemotherapy, a significant finding in efforts to tailor therapy to individual patients, according to a study published November 12 in the Journal of Nuclear Medicine.
Belgian researchers studied 37 patients with metastatic hormone-sensitive or castration-resistant prostate cancer who underwent gallium-68 (Ga-68) PSMA-11 PET/CT before and after rounds of taxane chemotherapy (docetaxel or cabazitaxel). They found patients whose tumors appeared to shrink on the second PET scan subsequently lived longer after a follow-up of two years.
"PSMA-PET response was independently predictive of survival with a statistically significant difference in [overall survival] between PSMA responders and nonresponders," wrote first authors Drs. Qaid Shagera and Carlos Artigas of the Free University of Brussels.
The U.S. Food and Drug Administration approved Ga-68 PSMA-11 in December 2020 for PET imaging of PSMA-positive lesions in men with prostate cancer. The technique has improved the diagnostic accuracy in initial staging of patients, yet few studies so far have explored using Ga-68 PSMA PET/CT for evaluating how patients respond to chemotherapy treatment.
"There is an unmet need to find a tool to evaluate, more timely and accurately, the response to chemotherapy" in cases of advanced prostate cancer, the researchers wrote.
In this study, the researchers retrospectively analyzed a database of all PSMA-PET/CT scans performed at their institution between January 2015 and May 2020. They analyzed data on 37 patients who underwent Ga-68 PSMA-11 PET/CT scans (Discovery 690 time-of-flight, GE Healthcare) within a median of 16 days before their first treatment and again within a median of 27 days after they completed the cycle. Twenty-one patients received docetaxel and 16 received cabazitaxel.
The researchers defined biochemical response as undetectable or decreased levels of prostate-specific antigen (PSA) by ≥50% compared to baseline, while a cut-off of ≥30% change in the total tumor volume on imaging for each patient defined treatment responders versus nonresponders.
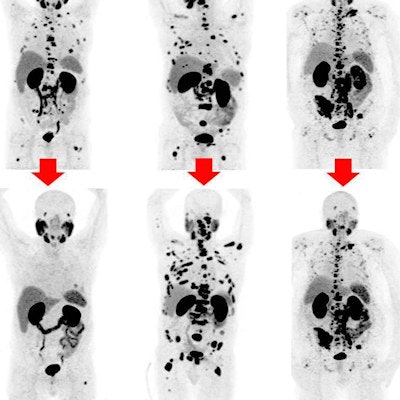
After analyzing the results, the researchers classified 18 of 37 patients as treatment responders (six with complete response and 12 with partial response) and 19 of 37 as nonresponders (17 with progressive disease and two with stable disease).
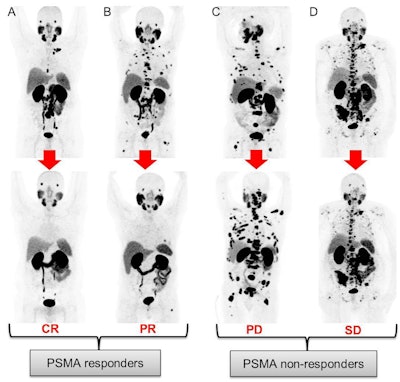 PSMA responders: patient (A) with the disappearance of all PSMA-positive lesions (complete response) and patient (B) with a decrease of PSMA-TV >30% (partial response). PSMA nonresponders: patient (C) with the appearance of new lesions and increased PSMA-TV >30% (progressive disease) and patient (D) with neither new PSMA-positive lesions nor PSMA-TV 30% changes (stable disease). Image courtesy of the Journal of Nuclear Medicine.
PSMA responders: patient (A) with the disappearance of all PSMA-positive lesions (complete response) and patient (B) with a decrease of PSMA-TV >30% (partial response). PSMA nonresponders: patient (C) with the appearance of new lesions and increased PSMA-TV >30% (progressive disease) and patient (D) with neither new PSMA-positive lesions nor PSMA-TV 30% changes (stable disease). Image courtesy of the Journal of Nuclear Medicine.After a median follow-up of 23 months, a total of 16 deaths had occurred. Among the whole population, responders identified on Ga-68 PSMA-11 PET/CT had longer overall survival compared to those identified as nonresponders (median overall survival not reached versus 12 months, hazard ratio 0.10), the researchers found.
"The PSMA-PET response was independently predictive of survival with a statistically significant difference in [overall survival] between PSMA responders and nonresponders," Shagera and Carlos Artigas wrote.
The role of PSMA-PET/CT for assessing treatment response has been reported in previous studies with promising results, yet the findings are preliminary and still inconclusive because of the heterogeneous treatment modalities considered and the lack of outcome data, the researchers noted.
Also, given the limited literature data on PSMA-PET/CT's role in assessing response to taxane-based chemotherapy in patients with metastatic prostate cancer, the results of this study warrant further investigations, they stated.
"Ga-68 PSMA-11 PET/CT is a promising imaging tool to assess response to taxane-based chemotherapy (docetaxel and cabazitaxel)" in prostate cancer patients, the researchers concluded.