Researchers have developed a clinical tool based on standard PET/CT imaging that could help cardiologists identify patients at high risk for heart attack and stroke, according to a study published online December 19 in the Journal of Nuclear Cardiology.
A group from Intermountain Medical Center Heart Institute in Salt Lake City, Utah, developed a PET/CT risk score to estimate the 90-day and one-year risk for patients for major adverse cardiac events (MACE) and revascularization. The tool proved highly predictive when tested and could help cardiologists improve patient outcomes, according to the team.
"As the overall health risk for a patient is important, using these risk scores might flag additional concerns for the cardiologist and perhaps drive additional assessment, treatment, and care," wrote corresponding author Stacey Knight, PhD.
Approximately 3.8 million patients undergo cardiac stress testing in the U.S. each year. Up to 15% of these tests result in false-negative results, with a significant percentage of these misdiagnosed patients subsequently experiencing major adverse cardiac events, including heart attack and death, the authors wrote.
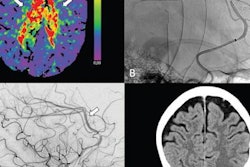
Cardiac PET/CT may reduce these misdiagnoses by providing higher image quality, according to the authors. Moreover, while PET has been around for decades, clinical use of cardiac PET/CT has been relatively limited, partly due to the steep learning curve involved in interpreting complex or ambiguous cases, the authors wrote.
In this study, the group gathered results from 11,552 patients who underwent PET/CT scans between 2015 to 2017 at their medical center. The patients were on average 65 years old, half were male, and a quarter had a prior heart attack or revascularization. The study authors culled imaging and clinical metrics such as ischemic burden (metrics on blood flow restrictions), coronary artery calcium, coronary flow reserve, smoking, and inpatient status to develop the model.
They then tested the model for estimating risk scores in patients in a separate set of PET/CT scans from 5,049 patients. They compared MACE-Revasc risk scores to risk based on conventional ischemic burden alone and the interpreting cardiologist's assessment of risk as documented in the official clinical interpretation of the scans.
The PET/CT 90-day MACE-Revasc risk score trended toward outperforming ischemic burden alone. The PET/CT one-year MACE-Revasc score was better than the use of ischemic burden alone, and both PET/CT MACE-Revasc risk scores outperformed risk prediction by cardiologists, according to the findings.
The results are promising and warrant validation in a different patient population, the researchers suggested.
"The use of these simple PET/CT MACE-Revasc risk scores in an external patient population should be examined as well as the determination of the value of their use in a clinical setting," the team concluded.