PET/CT imaging can serve as a metabolic guide to increase the accuracy of needle biopsies in patients with suspicious lung nodules, according to a study published January 18 in the European Journal of Radiology.
A team that included researchers in the U.K., Greece, and the U.S. studied whether F-18 FDG-PET/CT scans showing metabolic activity of suspicious nodules improved the accuracy of CT-guided biopsies, and the group recommended the approach based on the results.
“Our study showed that the availability of PET/CT prior to the [percutaneous needle lung biopsy] improves the diagnostic biopsy rates,” wrote lead author Konstantinos Stefanidis, MD, of King’s College Hospital in London, and colleagues.
CT-guided percutaneous needle biopsy is a minimally invasive procedure used to analyze tissue and is key in diagnosing suspicious pulmonary nodules, the authors explained. The accuracy of the procedure alone for identifying malignant tumors varies between 64% and 97%, and this is thought to be due to different levels of metabolic activity in the tumors, they added.
F-18 FDG-PET/CT is a molecular imaging approach that can locate maximum metabolic activity regions in tumors based on glucose metabolism by cancer cells. Yet there is no set guideline recommending PET/CT scans before CT-guided lung biopsy to assess the best site for obtaining tissue, the authors noted.
Thus, to provide further evidence that F-18 FDG-PET/CT can identify the most appropriate route and positioning of the biopsy needle, the group analyzed 340 consecutive cases of patients with suspicious lung nodules, masses, or extensive disease who underwent lung biopsy over a three-year period.
The researchers divided the cases into three groups: patients who had a PET/CT scan prior to the biopsy, those who had PET/CT following the biopsy, and those who did not undergo PET/CT. They then compared the accuracy of biopsies among the groups.
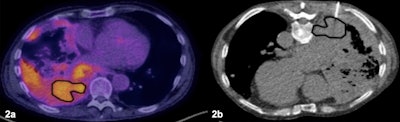 Patient with extensive lung and pleural disease. (2a) The PET/CT was available prior to the biopsy showing heterogeneous F-18 FDG radiotracer uptake and delineating the most accessible area of increased metabolic activity. (2b) The biopsy was targeted to the area of increased activity area and was positive for malignant diagnosis. Image courtesy of the European Journal of Radiology.
Patient with extensive lung and pleural disease. (2a) The PET/CT was available prior to the biopsy showing heterogeneous F-18 FDG radiotracer uptake and delineating the most accessible area of increased metabolic activity. (2b) The biopsy was targeted to the area of increased activity area and was positive for malignant diagnosis. Image courtesy of the European Journal of Radiology.
In total, 353 CT-guided lung biopsies were performed, with an overall diagnostic rate of 83.9 % (95.8 % malignant). The biopsy success rate was 88.8 % in the PET/CT prebiopsy group versus 78.9% in the group without PET/CT upfront, according to the findings.
Moreover, the biopsy success rate was 88.8 % when the biopsies targeted the PET/CT region showing the maximum tumor metabolic activity region, and only 52.8 % for biopsies that did not target these regions.
Finally, the researchers found that patients with a PET/CT prior to the biopsy underwent fewer needle passes (mean 2.6 vs. 3.1) required to obtain adequate sample sizes, they wrote.
“Metabolic information provided by F-18 FDG PET/CT and [percutaneous needle biopsy] localization to the PET/CT maximum activity region is associated with higher diagnostic biopsy rates, especially in masses, and appears to account for improved performance,” the group wrote.
Ultimately, radiologists should be encouraged to be aware that PET/CT images can improve the diagnostic accuracy of biopsies and contribute to early histologic diagnosis and staging, the group wrote.
“Our data clearly show the necessity to consider PET/CT as a metabolic guide in CT-guided biopsies and should be considered as a recommendation in future guidelines,” the group concluded.
The full article can be found here.