An international survey of treatment centers has revealed significant differences in several aspects of Lu-177 PSMA-617 prostate cancer therapy, including patient imaging protocols, according to a study published January 18 in the Journal of Nuclear Medicine.
Aligning these differences could improve patient outcomes, noted lead author Andrea Farolfi, MD, of the University of California, Los Angeles, and colleagues.
“Standardization or harmonization of protocols and dedicated training are desirable in anticipation of increasing numbers of patients and theranostic centers,” the group wrote.
Pluvicto was approved by the U.S. Food and Drug Administration (FDA) in March 2022 for adults with prostate specific membrane antigen (PSMA)-positive metastatic cancer who have not responded to standard treatments. While Pluvicto has been swiftly adopted into international prostate cancer management guidelines, identifying potential operational differences and similarities in how it is delivered can improve consistency of care, the authors noted.
To that end, the researchers sent a questionnaire comprising 62 items to 211 Pluvicto treatment centers globally in June 2022. They received 95 (45%) responses, with participants asked to provide answers about how patients are imaged and treated.
Most participating centers were in Europe (51%), followed by the U.S. (22%) and Asia (22%), the group wrote. During the 12 months before the study, a total of 5,906 patients received Pluvicto therapy at the 95 participating centers.
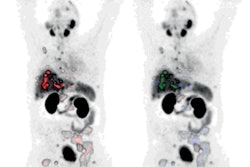
The researchers highlighted several variations. For instance, while the FDA advises that selection of patients for treatment be made using an approved PSMA radiotracer and based on tracer uptake in tumors, they found that most commonly, subjective visual whole-body PSMA-PET scans were performed (33%).
In addition, different PET radiotracers are used. Gallium-68 (Ga-68) PSMA-11 was the most frequently used PET radiotracer (77%), followed by F-18 PSMA-1007 (41%), Ga-68 PSMA-I&T (22%), and F-18 DCFPyL (19%).
At 12 centers, technetium-99m (Tc-99m)-labeled PSMA for SPECT imaging was sufficient to assess patient eligibility, and these locations were predominantly in Germany (5), Iran (2), and Mexico (2), the researchers noted.
Moreover, administered doses in the survey ranged between 5.5 and 11.1 GBq, the researchers wrote. More than half the centers (53%) adapted the injected dose on the basis of the patient’s bone marrow, salivary gland, kidney, or liver function, while dose deescalation or adaptation based on patient weight or dosimetry was performed at fewer than 12% of centers, according to the findings.
“Results from this international survey revealed interinstitutional differences in several aspects of Lu-177 PSMA radionuclide therapy,” the group wrote.
Ultimately, the variation seen in the responses reflect differences in accepted practice standards in different countries and may be supported by evolving clinical practice guidelines, the researchers wrote.
“Some responses, however, raise concern and highlight the need for theranostic centers, specific training, and an improved evidence base as theranostics is widely adopted,” they concluded.
A link to the full article can be found here.