A radiomics nomogram based on F-18 FDG-PET/CT imaging could help clinicians assess long-term outcomes in women undergoing treatment for locally advanced cervical cancer, according to a study published January 30 in BMC Cancer.
The nomogram was tested in women who had undergone radiochemotherapy and effectively predicted 3-year and five-year progression-free survival outcomes, noted co-corresponding author Ruozheng Wang, PhD, of Xinjiang Medical University in Urumuqi, China.
“The nomogram incorporating radiomics and clinical features could be a useful clinical tool for the early and accurate assessment of long-term prognosis in patients,” the group wrote.
Cervical cancer is the fourth most frequent cause of cancer-related morbidity and mortality in women worldwide, especially in developing countries, the authors noted.
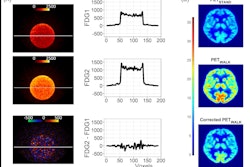
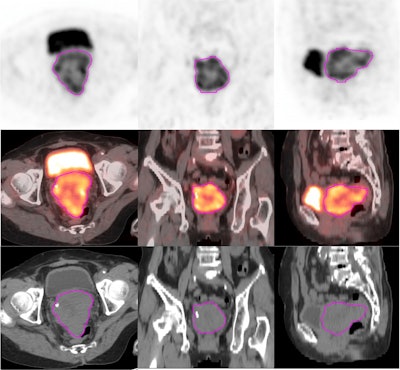
While conventional medical imaging approaches provide information related to the tumor structure and facilitate diagnoses in these patients, radiomics – an approach based on extracting quantitative data from images to generate imaging biomarkers – could help determine whether patients are responding to treatment, they added.
To that end, the group analyzed data from 167 patients with locally advanced cervical cancer (LACC) who underwent pretreatment F-18 FDG PET/CT and radiochemotherapy at two local cancer centers. They extracted radiomics features from this data based on their clinical effectiveness in predicting 3- and 5-year progression-free survival.
In a separate cohort of 117 patients, in total, one clinical, one PET radiomics, and three CT radiomics features were significantly associated with progression-free survival, according to the findings. Next, in a cohort of 50 patients, the researchers found that a model that combined these features was better at predicting progression-free survival than any of the parameters alone.
Finally, in a cohort of 23 patients from another hospital, the nomogram predicted 3-year progression-free survival (PFS) in patients with LACC with an area under the operating curve (AUC) of 76% and 5-year PFS with an AUC of 68%, according to the findings.
“We successfully developed a combined risk stratification model that incorporated clinical, PET radiomic, and CT radiomic features for individual prediction of 3- and 5-year PFS probability in patients with LACC who received definitive concurrent radiochemotherapy,” the group wrote.
Ultimately, the study is of clinical value, as is provides a visually quantitative nomogram to aid clinicians in their routine practice, the authors wrote. Yet they noted limitations, namely that a longer follow-up is needed to further established the value of the nomogram.
“Future prospective studies including more clinical parameters and several clinical endpoints need to be performed to further validate and enhance the predictive performance,” the group concluded.
The full article can be found here.